Blocking Sleep-Wake Protein Orexin May Treat Alzheimer’s
 Researchers from the School of Medicine at Washington University in St. Louis (WUSTL) blocked a sleep-regulating protein, orexin, in mice with a form of Alzheimer’s disease, making them sleep longer and blocking brain symptoms of Alzheimer’s disease. The research appeared Nov. 24 in The Journal of Experimental Medicine.
Researchers from the School of Medicine at Washington University in St. Louis (WUSTL) blocked a sleep-regulating protein, orexin, in mice with a form of Alzheimer’s disease, making them sleep longer and blocking brain symptoms of Alzheimer’s disease. The research appeared Nov. 24 in The Journal of Experimental Medicine.
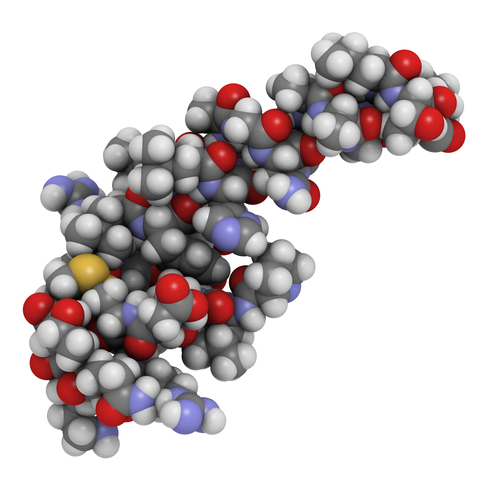
In Alzheimer’s disease, a sticky protein known as amyloid-β (Aβ) clogs up the brain, killing brain cells (neurons), disturbing memory and also disrupting the sleep-wake cycle. The accumulation of Aβ in the brain forms plaques, a hallmark of Alzheimer’s disease.
Also known as hypocretin, orexin is a molecule that controls wakefulness, as well as eating, motivation, and emotion. Orexin is thought to be important for maintaining regular sleep patterns. People with low orexin can have narcolepsy — a condition associated with sleeping excessively. Levels of orexin in the cerebrospinal fluid have recently been found to be decreased in Alzheimer’s disease, and these decreases correspond abnormal sleep patterns.
According to an author of the study, David M. Holtzman, MD, head of the Department of Neurology, “If you stimulate orexin production in sleeping mice, they wake up immediately.”
The scientists took mice that had been genetically modified to over-produce Aβ, creating a form of Alzheimer’s disease. They also blocked the gene for orexin. Blocking the orexin gene reduced the build-up of Aβ that occurs in the brains of these Alzheimer’s-like mice by about 50%. It also made the mice sleep more. When the researchers tried the opposite experiment, to increase orexin levels, the mice developed more Aβ plaques and were awake longer.
In a third type of experiment, the researchers blocked orexin only partially, so that they did not affect the amount of time mice slept. This did not have any effect on Aβ plaque accumulation.
According to Holtzman, “The results from this new paper demonstrate that the absence of orexin results in a marked decrease in amyloid-beta accumulation in the brain. The data strongly suggest that the effect of orexin on amyloid-beta is due to orexin’s effect on sleep. The implications are that under certain circumstances, increasing sleep by as little as 10% might be able to strongly decrease amyloid-beta accumulation. This could mean that if sleep was changed during mid adult life to such an extent, in the long run, it might be able to significantly delay the onset of amyloid accumulation and pathology and later on the cognitive decline of Alzheimer’s disease.”
The researchers, including first author Jee Hoon Roh, MD, PhD, are now studying the effects of sleep medications on Aβ production and plaque build-up in the Alzheimer’s diseased brain.
Holtzman remarked, “Experiments we are pursuing now include assessing the effects of sleep disruption on dynamic regulation of amyloid-beta in humans as well as whether the presence of AD pathology during the period of preclinical AD is associated with disrupted sleep.”