Is Iron In The Brain Of Alzheimer’s Patients?
Stanford University School of Medicine researchers have found microglia containing iron in the brains of people with Alzheimer’s disease (AD), a condition not verified in the brains of healthy people. The iron-containing cells appeared in the hippocampus, a critical area for memory that also degenerates in AD. The work appeared in the journal Neurobiology of Aging.
Beta-amyloid protein and another form of protein called hyperphosphorylated tau have been suspected causes of AD for decades. The study does not exclude that these proteins could cause AD, but it adds another culprit to the mix of things that can cause AD and brain degeneration.
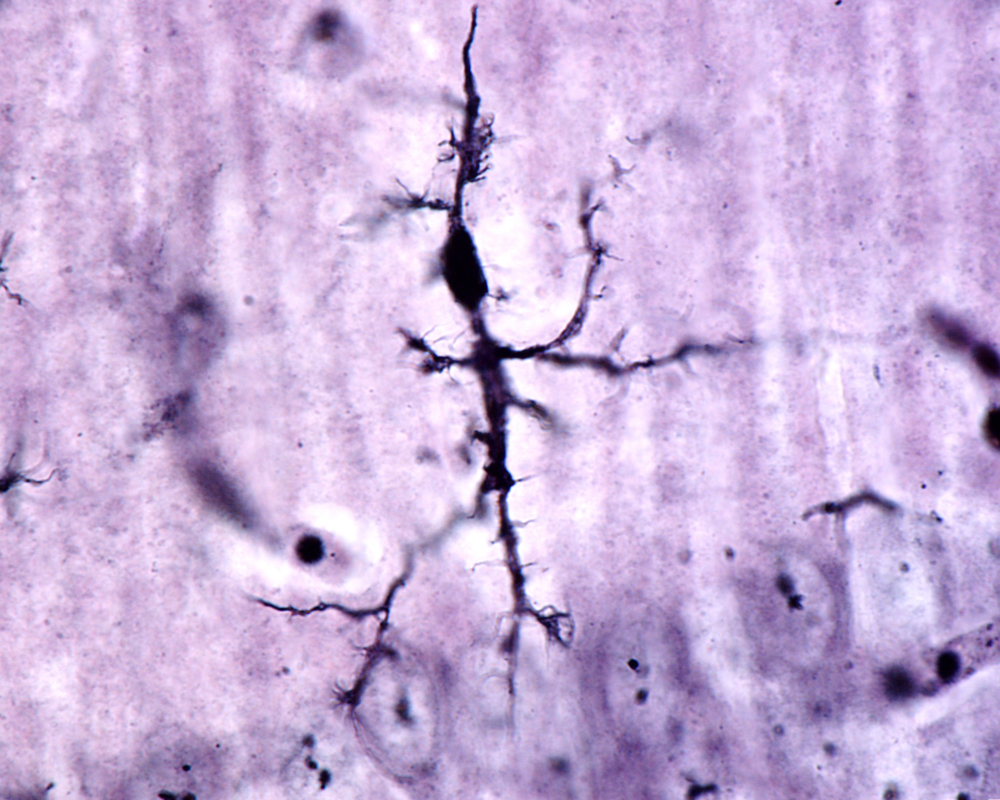
The scientists were able to identify microglia, considered the immune system of the brain, with iron in the brains of people with AD who had died, by using a unique type of brain imaging technique known as high-field magnetic resonance imaging (using a specialized version called 7T MRI). This form of MRI might be used to diagnose AD in the future.
The investigators studied a total of five brains of people with AD and compared it to five healthy brains. “Microglia are the brain’s immune cells,” noted Michael Zeineh, MD, PhD, assistant professor of neuroradiology and the lead study author. The cells can exist in different states and have a different phenotype depending on whether they are “resting” or “activated.” In an activated state they may fight off infection or disease, but can also become over-activated and cause damage. Most of the iron-containing microglia found in this study were in an activated state.
These studies in human brains are supported by earlier mouse studies. Senior author, Brian Rutt, PhD, professor of radiology, remarked “Some imaging studies using mouse models of Alzheimer’s disease had revealed the presence in these mice’s brains of tiny, mysterious black dots that could signal the presence of iron, an element that shows up dark under MRI and, in certain chemical forms, can be highly reactive and inflammation-inducing. We wanted to see if there was an association of iron with Alzheimer’s plaques in humans”.
Interestingly, the iron-containing microglia in human brain did not consistently appear in association with other hallmarks of AD, beta-amyloid and tau. Beta-amyloid typically forms deposits known as plaques. “We didn’t consistently find the iron associated with plaques as we were expecting, despite our best efforts to do that,” noted Rutt.
The next step for these scientists will be to use neuroimaging to look for iron in AD brains at earlier stages of the disease in living individuals, to help further assess whether iron can be used as a biomarker for AD diagnosis.






