Alzheimer’s Transition from Asymptomatic to Dementia May Be Foreseen in a Protein Biomarker
Researchers in Germany have identified a potential brain inflammation biomarker in the cerebrospinal fluid of patients with early and asymptomatic Alzheimer’s disease. This biomarker may help clinicians identify Alzheimer’s at its transition stage from preclinical disease to cognitive impairment and dementia progression. The research, titled “sTREM2 cerebrospinal fluid levels are a potential biomarker for microglia activity in early‐stage Alzheimer’s disease and associate with neuronal injury markers,” was published in EMBO Molecular Medicine.
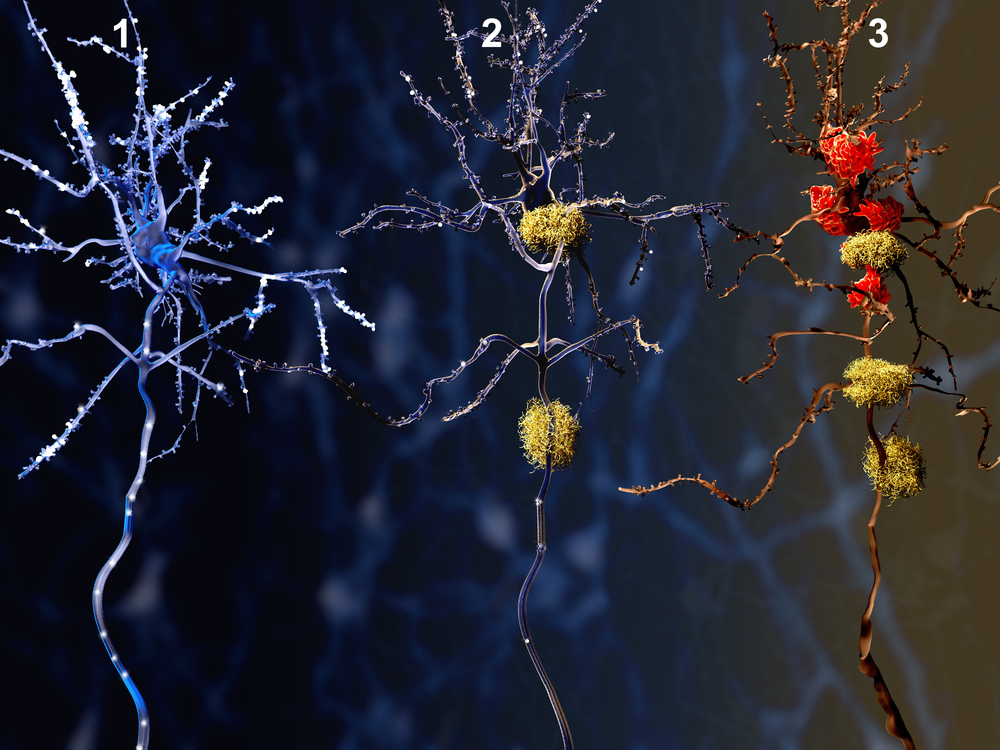
Two of Alzheimer’s disease (AD) hallmarks, amyloid peptide plaques and tau protein aggreagates, are often used as preclinical diagnostic markers. However, the diagnostic measure of these structures in the cerebrospinal fluid has low specificity, because an individual can present these anomalies but maintain cognitive abilities for several years post-diagnosis. Early and accurate diagnosis of AD could increase treatment options for patients and facilitate clinical trials of new therapeutic agents, so research greatly focuses on the discovery of early disease biomarkers. In previous studies, researchers have shown that the loss of the function of the protein TREM2, an innate immune receptor expressed on the surface of microglia, impairs the defense abilities of microglial cells, reducing the clearance of amyloid plaques. Such observations have led researchers to believe that TREM2 may play an important role in the pathogenesis of AD and the onset of neurodegeneration.
Researchers in this multicenter study focused on the TREM-2 protein and its role in the initial protective inflammation that occurs in AD. A large set of patients with different levels of cognitive impairment and different stages of Alzheimer’s were included, and researchers measured the levels of secreted TREM-2 in patients’ cerebrospinal fluid. Results showed that during the earlier stages of the disease, characterized by mild cognitive impairment, TREM-2 levels were high. In contrast, the protein’s levels were lower in more advanced stages of AD with full dementia, a pattern that closely mirrors the microglia activity during disease course. Researchers believe these findings suggest microglia-mediated brain inflammation marks the transition between early stage preclinical AD and full dementia.
“We now have the first marker for the capacity of brain immune cells to remove toxic materials,” Dr Christian Haass with the German Center for Neurodegenerative Diseases (DZNE), and one of the study’s lead authors, said in a press release, “and its increase long before full Alzheimer’s dementia shows that there is early neuronal injury that does not yet affect memory, but already triggers a microglia response.”
“If this response is indeed protective, then therapeutically modulating the activity of microglia could be beneficial in late-stage Alzheimer’s patients as well as other brain disorders,” added Dr. Michael Ewers, with the Institute for Stroke and Dementia Research in Munich.






