MIT Team Reveals What Happens to Brain Immune Cells During Alzheimer’s Development
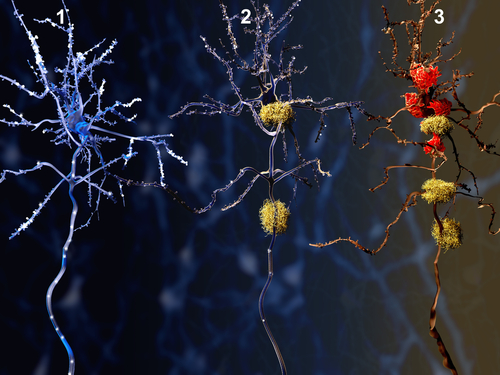
Massachusetts Institute of Technology researchers have found that Alzheimer’s disease causes microglia — the immune cells that normally protect brain cells from damage — to change their behavior and instead promote a pro-inflammatory immune response.
Their study, “Temporal Tracking of Microglia Activation in Neurodegeneration at Single-Cell Resolution,” appeared in the journal Cell Reports.
“Right now, microglia are really in the spotlight for a number of neuro-system diseases, including Alzheimer’s, and also schizophrenia,” Li-Huei Tsai, director of MIT’s Picower Institute for Learning and Memory and the study’s senior author, said in a news release. “However, there are still a lot of very basic things that we don’t know about microglia, such as whether cells in the healthy and diseased brain are all the same, or whether there are different groups, and how they become more inflammatory in the diseased state.”
Microglia cells have been linked to several neurodegenerative disorders including Alzheimer’s. However, researchers know little about how this process is regulated.
Using the latest technology, the MIT team analyzed the gene expression profiles of individual microglia cells collected from the brains of mice with Alzheimer’s like-disease. The animals were engineered in Tsai’s lab to have a protein called p25 in the brain, which, when activated, triggers symptoms similar to those observed in humans with Alzheimer’s.
Researchers analyzed the gene expression just before activating p25 protein, and one week, two weeks and six weeks after activation.
“This allowed us to follow how microglia respond to the progression of the disease, and the worsening conditions in the mouse brain,” said Hansruedi Mathys, postdoc researcher at the Picower Institute and lead author of the study.
The team observed that microglia cells started to change their behavior within just a week. They began proliferating more than microglia cells collected from control animals that were not modified to develop Alzheimer’s like-disease. This finding suggests that microglia cells are able to sense perturbations in the mouse brain at a very early time point, said Mathys.
When the team looked at cells in later timepoints of disease development, they saw that the cells stopped proliferating and began to express more genes related to pro-inflammatory signals and activation of an immune response.
“The microglia initially transition from a resting state into a proliferation state, after which they transition again into a mainly inflammatory state, with very high expression of genes with a very specific immune system function,” Tsai said.
Researchers also identified different groups of microglia cells that expressed specific patterns of gene expression linked to distinct roles in immune response. This suggests that microglia can regulate several mechanisms involved in neurodegeneration and Alzheimer’s development. However, further studies are needed to test this hypothesis, which may lead to potential new targets for drug discovery.
“I find it particularly exciting that cells transition through different phases, seemingly following different gene expression programs,” said Tony Wyss-Coray, professor of neurology and neurological sciences at Stanford University. “This confirms the suspicion that there is a lot of cellular heterogeneity in microglial response to damage, but this paper actually shows this for the first time in a temporal fashion.”






