Texas A&M and Celltex Partnering on a Stem Cell-related Alzheimer’s Treatment
Written by |
Texas A&M’s Institute for Regenerative Medicine and Celltex Therapeutics are teaming up to evaluate whether inflammation-fighting sacs that stem cells release could be used to treat Alzheimer’s.
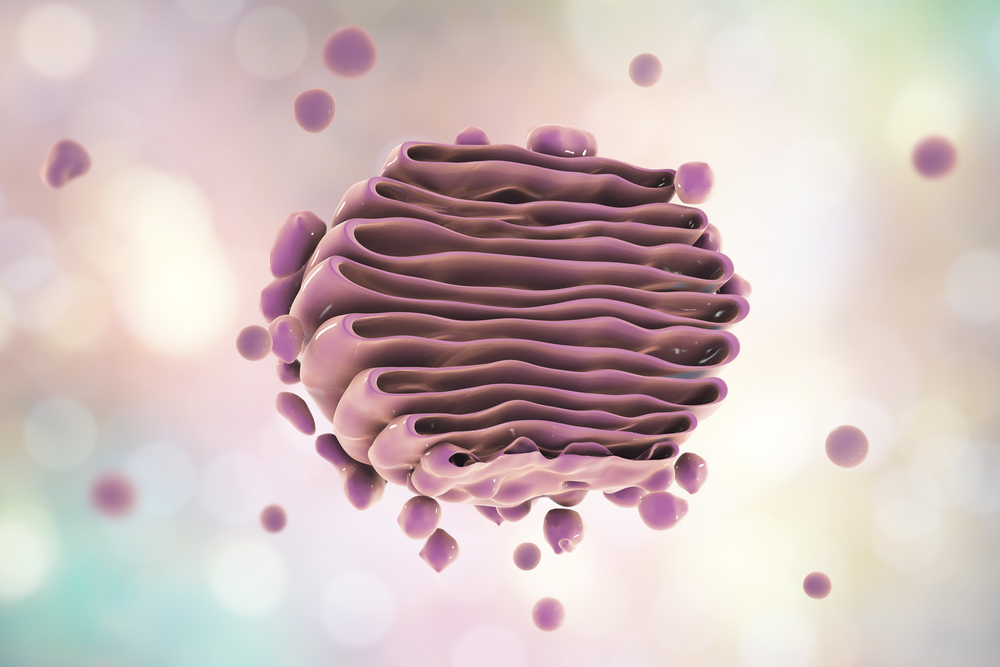
The fluid-filled sacs, which scientists call vesicles, transport material inside a cell. But cells often release them, and when this happens, they are called exosomes.
Researchers at Texas A&M and Celltex plans a multiyear study on whether inflammation-fighting mesenchymal stem cell exosomes can be used to treat Alzheimer’s. Mesenchymal stem cells can develop into almost any type of cell in the body, including bone, cartilage, muscle and fat.
The initial studies will involve animals, but the goal is to have clinical trials in humans within three years.
Exosomes are found in many body fluids, including blood and urine. They have specialized functions, including playing a key role in cell-to-cell signaling. These specialty roles give them great potential as therapies, including delivering anti-inflammatory agents to the brain.
“We are hopeful that this research might someday treat the disease [Alzheimer’s] effectively by stopping or delaying the neuronal [nerve cell] damage,” Dr. Ashok K. Shetty, associate director of the Institute for Regenerative Medicine, said in a Texas A&M news story. “Alternatively, exosomes may rejuvenate the networks of surviving but sick neurons via anti-inflammatory and neuroprotective effects.”
Dr. Darwin J. Prockop, the director of the Institute for Regenerative Medicine, will use mesenchymal stem cells to generate the exosomes for the project. Shetty will test their ability to reduce brain inflammation and help repair the nerve cell damage seen in Alzheimer’s.
Celltex’s contribution to the work will be its proprietary process for generating unprecedented levels of mesenchymal stem cells. The stem cells that the process generates are used to treat autoimmune, blood vessel, and degenerative diseases — and injuries.
Prockop and Shetty have already worked together on research dealing with exosomes’s capacity to decrease brain damage from injuries and seizures.
One of their discoveries was that exosomes could limit a prolonged type of seizure’s damage to the brain.
The study in animals involved a seizure disorder called status epilepticus that lasts 30 minutes or longer. It consists of a series of seizures in which a person fails to regain consciousness between episodes. If not quickly addressed, it can lead to brain damage, loss of cognitive function and loss of memory.
The brain inflammation these seizures generate is similar to that seen in the late stages of other brain diseases, including Alzheimer’s.
Prockop and Shetty used a nasal spray to administer the anti-inflammatory exosomes. The treatment eased nerve cell inflammation and prevented cognitive and memory dysfunction. It also stopped abnormal nerve cell generation in the hippocampus, the part of the brain responsible for memory.
“My laboratory has done research for over 20 years on the adult stem cells that are called MSCs [mesenchymal stem cells] and that Celltex has developed,” Prockop said. “Recently, we and others discovered that many of the beneficial effects of MSCs are caused by the small vesicles called exosomes that MSCs secrete.
“The agreement with Celltex is based on our more recent discovery that we can use MSCs to produce large amounts of a specific kind of exosomes that reduce inflammation, which is a process by which the body tries to repair injured tissues,” Prockup added.
“Unfortunately, inflammation is excessive in many diseases, and actually does the opposite and increases the damage to tissues,” he said. “However, we found that our anti-inflammatory exosomes decreased tissue damage in several animal models for human diseases, including diseases of the brain. The results strongly suggest the exosomes can provide a new and effective therapy for Alzheimer’s disease.”
Healthcare experts estimate that more than five million Americans have Alzheimer’s.
“Right now, there is no cure,” Shetty said. “The best that drugs can do is conceal the cognitive and behavioral symptoms of Alzheimer’s in the short term, but they do not cure the underlying disease or halt its advancement. We are hopeful that this research might some day treat the disease effectively by stopping or delaying the neuronal damage. Alternatively, exosomes may rejuvenate the networks of surviving but sick neurons via anti-inflammatory and neuroprotective effects.”





