Protein Involved in Calcium Transport in Nerve Cells Linked to Alzheimer’s in Early Study
Written by |
A protein that’s involved in calcium transport within nerve cells was linked to sporadic Alzheimer’s disease by scientists working in Spain. This protein, called STIM1, may hold promise as a biomarker of this common and non-familial form of Alzheimer’s.
Importantly, common treatments for hypertension that are based on dihydropyridine — and known as calcium channel blockers — were seen to halt nerve cell death in a laboratory setting.
The study, “STIM1 deficiency is linked to Alzheimer’s disease and triggers cell death in SH-SY5Y cells by upregulation of L-type voltage-operated Ca2+ entry,” was published in the Journal of Molecular Medicine.
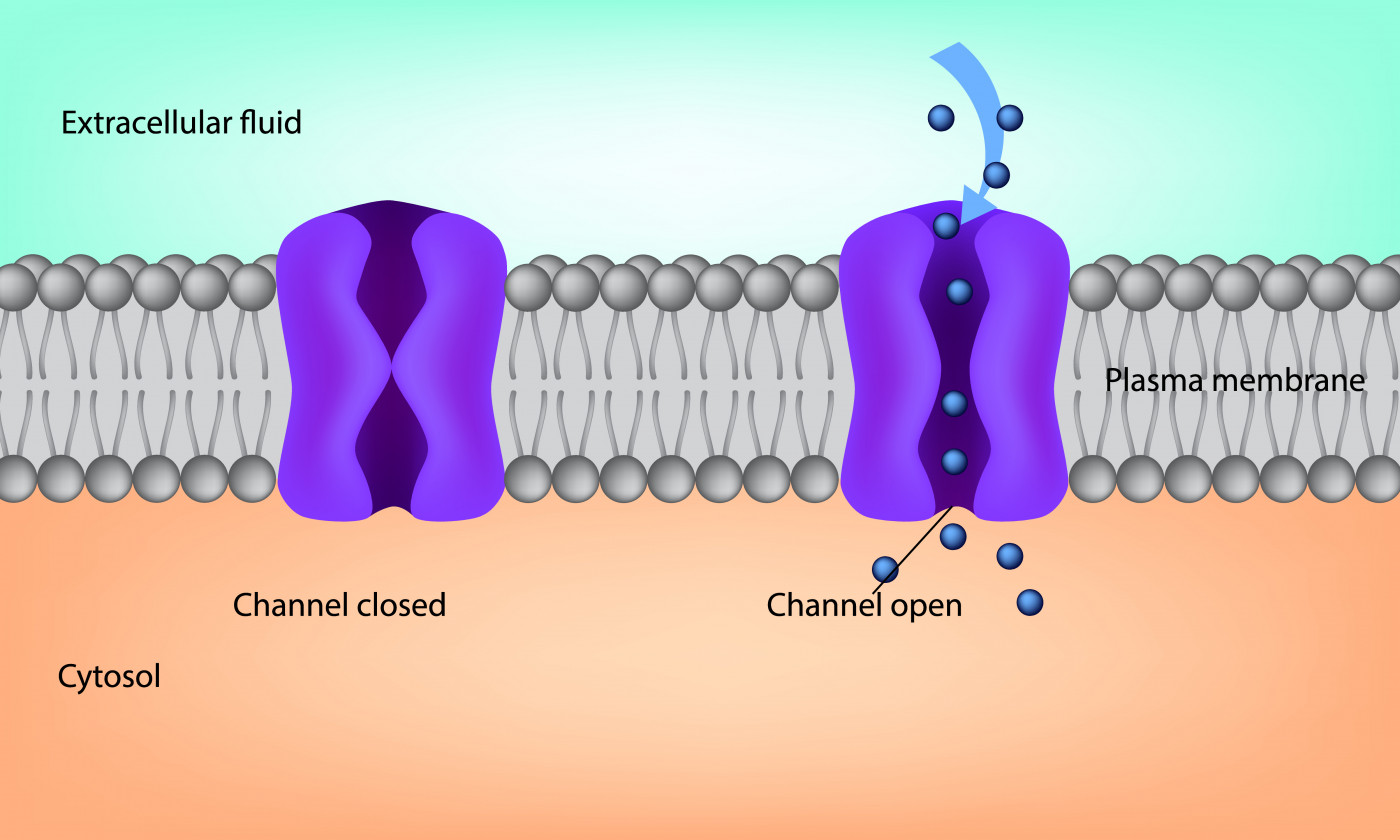
STIM1 is a protein found in the endoplasmic reticulum, a structure whose responsibilities include storing calcium in cells. STIM1 plays an important role on calcium uptake by regulating the activity of calcium channels (transporters) that exist in cell membranes.
Calcium is a key element for the proper working of all the cells in our body. In the brain, calcium dysregulation is a known cause of sporadic Alzheimer’s.
Most cases (95%) of Alzheimer’s disease occur in a sporadic, or unknown, way. Only 5% of all cases are due to a genetic cause.
Although STIM1 had already been associated with calcium regulation, a direct link between this protein and Alzheimer’s had not been studied.
Researchers at Universidad de Extremadura (UEx) in Spain analyzed cultures of human brain tissue affected by the neurodegeneration associated with this common form of Alzheimer’s.
The tissues, supplied by the Netherlands Brain Bank, derived from a brain region called medium frontal gyrus — part of the brain’s frontal lobe. They were from six confirmed Alzheimer’s patients and six age-matched patients with clinically-diagnosed non-Alzheimer’s degenerative conditions.
By comparing these two groups of samples, researchers were able to identify a deficiency in the STIM1 protein in brain tissue from Alzheimer’s patients.
“We have been working with this protein for 10 years, but we weren’t expecting these results with sporadic Alzheimer’s,” Francisco Javier Martin-Romero, a study author, said in a press release.
To confirm the involvement of STIM1 in neurodegeneration, the team used the CRISPR/Cas9 gene editing system, which works as a kind of “genetic cut-and-paste” tool. CRISPR technology allows scientists to edit genomes with precision and efficiency in the lab, but is not generally thought ready for use in patients.
The tool was used to eliminate the STIM1 gene from the DNA of a neuroblastoma (a type of nerve cell cancer) cell line, called SH-SY5Y cells, to recreate what happens in sporadic Alzheimer’s disease. Then, the behavior of the STIM1-deficient cells was evaluated.
“CRISPR silences the gene which permits the expression of the protein STIM1 in the neuron. Thus, we were able to simulate what occurs in the neuron without this protein, and we observed alterations very similar to those seen in tissues with Alzheimer’s,” Martin-Romero said.
One of the alterations seen in STIM1-deficient cells was in calcium transport across the cell membrane of the neural cell line.
“This calcium is necessary for the cell to be fully viable, and an alteration in this process affects its entire physiology, finally causing death. The cell is unable to halt the transport of calcium, which becomes unregulated and out of control,” he added.
Calcium transport through the calcium channels is mediated by a voltage. The activity of such voltage-gated calcium channels can be blocked using available calcium channel blockers based on dihydropyridine — a finding of potential importance in treating Alzheimer’s.
“[T]he results prove that [calcium channel] upregulation is essential to trigger cell death in STIM1-deficient cells, a proposal that fits well with the protective effect of dihydropyridines against neurodegeneration in AD [Alzheimer’s disease] patients,” the researchers wrote.
STIM1 levels may also serve as a biomarker of disease progression, they added.





