Targeting Single Enzyme May Produce Multiple Benefits for Alzheimer’s, Mouse Study Suggests
Written by |
Targeting a single enzyme called PI3K-delta prevented neuroinflammation, reduced the accumulation of toxic amyloid-beta plaques in the brain, and prevented memory deficits in a mouse model of Alzheimer’s disease, a new study shows.
This approach, which also increased the animals’ life span, may represent a potential new strategy to halt Alzheimer’s progression and ease hallmark symtoms of the disease.
The study, “p110δ PI 3-kinase inhibition perturbs APP and TNFα trafficking, reduces plaque burden, dampens neuroinflammation and prevents cognitive decline in an Alzheimer’s disease mouse model,” was published in the Journal of Neuroscience.
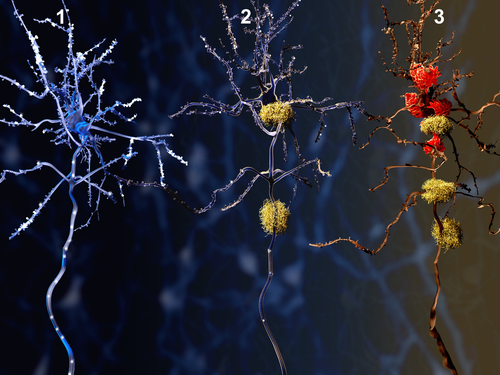
Accumulation of abnormal amyloid-beta aggregates in brain cells and activation of microglia — the resident immune cells in the brain — are two key features of Alzheimer’s.
Amyloid-beta protein accumulation is considered one of the main triggers of Alzheimer’s. Its deregulation and progressive deposition promotes the activation of microglia, which can be beneficial in the early stages of Alzheimer’s by helping to prevent the spreading of plaques. However, chronic microglia activation and neuroinflammation ultimately leads to nerve cell death and cognitive decline.
As researchers investigate the processes underlying Alzheimer’s disease, they say it may be necessary to target both neurological and inflammatory components at the same time.
“Most treatments focus on only one aspect of the disease; we want to change this point of view and focus on developing therapies that touch different aspects of the disease, like the combined approaches used to treat cancer,” Ramón Martínez-Mármol, PhD, lead author of the study and researcher at Queensland Brain Institute , in Australia, said in a news release.
With this in mind, Australian and U.K. researchers used a mouse model of Alzheimer’s to explore the role of the enzyme PI3K-delta, an important regulator of pro-inflammatory signals from immune cells. It is also found in neurons, although its role there remains not well understood.
Results showed that mice carrying a mutation that inactivates PI3K-delta produced lower levels of amyloid-beta and plaques in comparison to animals with the normal enzyme. Inactivation of PI3K-delta also abolished inflammatory responses and decreased the transporter of amyloid precursor protein (APP) — the precursor molecule whose breakdown generates amyloid-beta — in nerve fibers.
Importantly, animals with inactivated PI3K-delta also showed no memory or learning deficits, and had a normal life span.
“We were surprised to find that having none of the [normal] enzyme in their system … [the mice] didn’t have Alzheimer’s disease at all — the mice were completely normal with intact memory,” Martínez-Mármol said.
Next, the researchers tested the impact of CAL-101 — a selective PI3K-delta inhibitor marketed with the brand name Zydelig (idelalisib, by Gilead) for the treatment of B-cell lymphoma — in the nerve cells and microglia collected from mice with Alzheimer’s.
Treatment with CAL-101 significantly reduced the transport of APP inside neurons, likely decreasing its conversion to amyloid-beta and preventing its deposition and toxic effects. It also significantly eased the release of the strong pro-inflammatory molecule TNF-alpha by microglia cells.
“We conclude that inhibiting PI3K [delta] represents a novel therapeutic approach to ameliorate [Alzheimer’s] pathology by dampening plaque accumulation and microglial-dependent neuroinflammation,” the researchers wrote.
Despite the potential of this dual-effect approach for treating Alzheimer’s, more work is still required to translate it to patients. CAL-101 showed effectiveness in vitro, but is not able to cross the blood-brain barrier to reach the brain.
“We are now keen to collaborate with other researchers to work out how to solve the issue of transporting the drug across the blood-brain barrier,” Martínez-Mármol said.





