Alzheimer’s Disease Appears to Be Driven by Brain Inflammation
Written by |
British researchers recently identified a protein driving brain inflammation, CSF1R, which they think may be the driving force behind the progression of Alzheimer’s disease (AD).
The study, “Pharmacological targeting of CSF1R inhibits microglial proliferation and prevents the progression of Alzheimer’s-like pathology” and published in the journal Brain, could be a significant step forward in the understanding of mechanisms contributing to Alzheimer’s pathology.
Researchers long suspected that inflammation is involved in AD, but have been less certain as which is “the hen” and which is “the egg” — i.e., is the pathology driving inflammation, or vice versa. However, Adrian Olmos-Alonso and colleagues from the University of Southampton, U.K., clearly show that inflammation is driving pathology in AD.
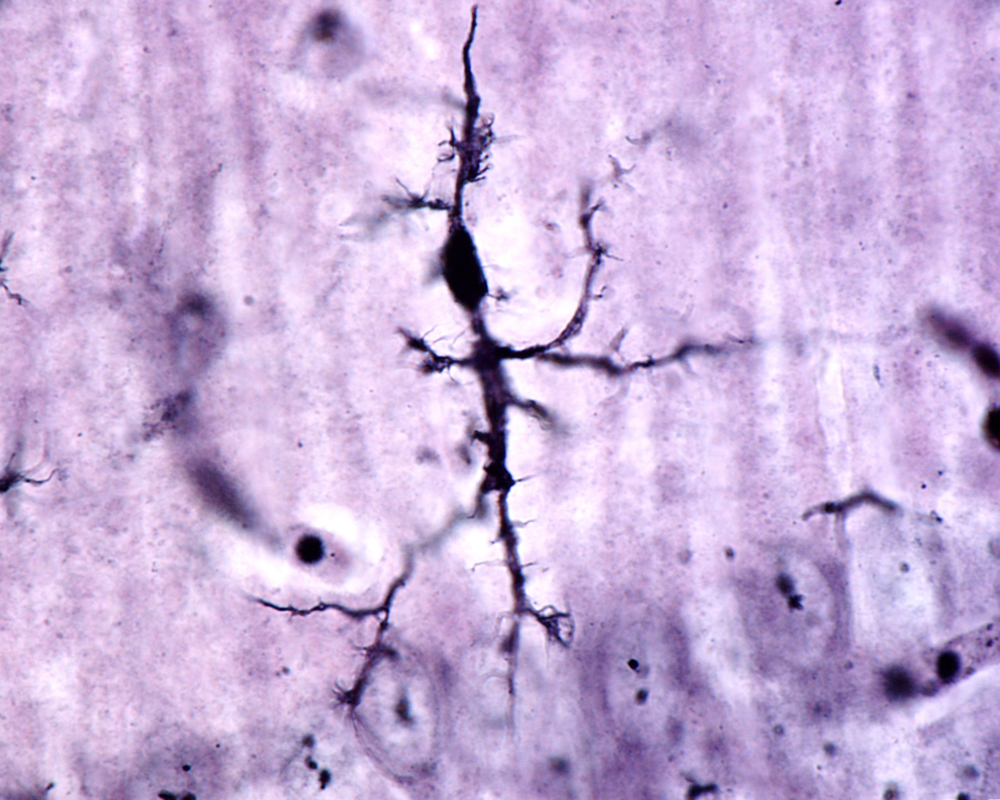
Researchers found that AD patients’ brains harbored increased numbers of microglia, or brain immune cells. There were also signs of an increased expansion rate of microglia, and the team noticed that the cells displayed high expression of many inflammatory genes — in particular, they saw significant increases in the CSF1R pathway, a receptor for CSF1, an immune molecule responsible for the production and function of microglia.
To investigate the effects of CSF1R in more detail, the team used a mouse model of AD. They observed a similar increase in the number of microglial cells in AD mice, which became more abundant in older animals and were multiplying close to β-amyloid plaques. They also noticed that the levels of the protein CSF1R were increasing in the same way, along with other inflammatory genes associated with microglial activation.
When mice were treated with a drug blocking the CSF1R receptor, the microglia stopped proliferating and dropped in number. The detail making this finding stand out is that the drug did not remove all the microglial cells — it merely restored their numbers to the level seen in normal mice.
The reduced numbers of microglia also led to a reduction in other inflammatory molecules, and — more importantly — to improved memory and other disease-related behavior in the mice.
The drug also restored synaptic connections between neurons; however, it did not remove the β-amyloid plaques. This indicates that plaque formation alone is not sufficient to cause disease. Rather, inflammation is needed for the development of AD symptoms.
The authors hope their findings may lead to the development of drugs targeting CSFR1 as an AD treatment.
In a press release, Dr. Diego Gomez-Nicola, who led the study, said, “These findings are as close to evidence as we can get to show that this particular pathway is active in the development of Alzheimer’s disease. The next step is to work closely with our partners in industry to find a safe and suitable drug that can be tested to see if it works in humans.”
Dr. Rob Buckle, director of science programs at the Medical Research Council, added, “It is increasingly clear that inflammation is a key player in a number of neurodegenerative conditions, and this study is beginning to unravel the biological processes behind this link.”





