Synaptic Loss Precedes Alzheimer’s Symptoms and Drives Disease, New Study Finds
Before any signs of cognitive decline start showing, neuronal synaptic connections are lost in mice destined to develop Alzheimer’s. New research shows that microglia – brain immune cells – destroy synapses in a fashion resembling processes in the developing brain, suggesting that it might be possible to develop drugs targeting disease at far earlier stages.
The process of synaptic pruning – the loss of neuronal connections – is crucial for producing distinct neuronal circuits during normal brain development. When synapses are not successfully eliminated, conditions such as autism might arise. Excessive pruning has also been suggested to contribute to psychiatric conditions such as schizophrenia. It is easy to envision how disruption of these developmental processes might lead to disease in children and adolescents.
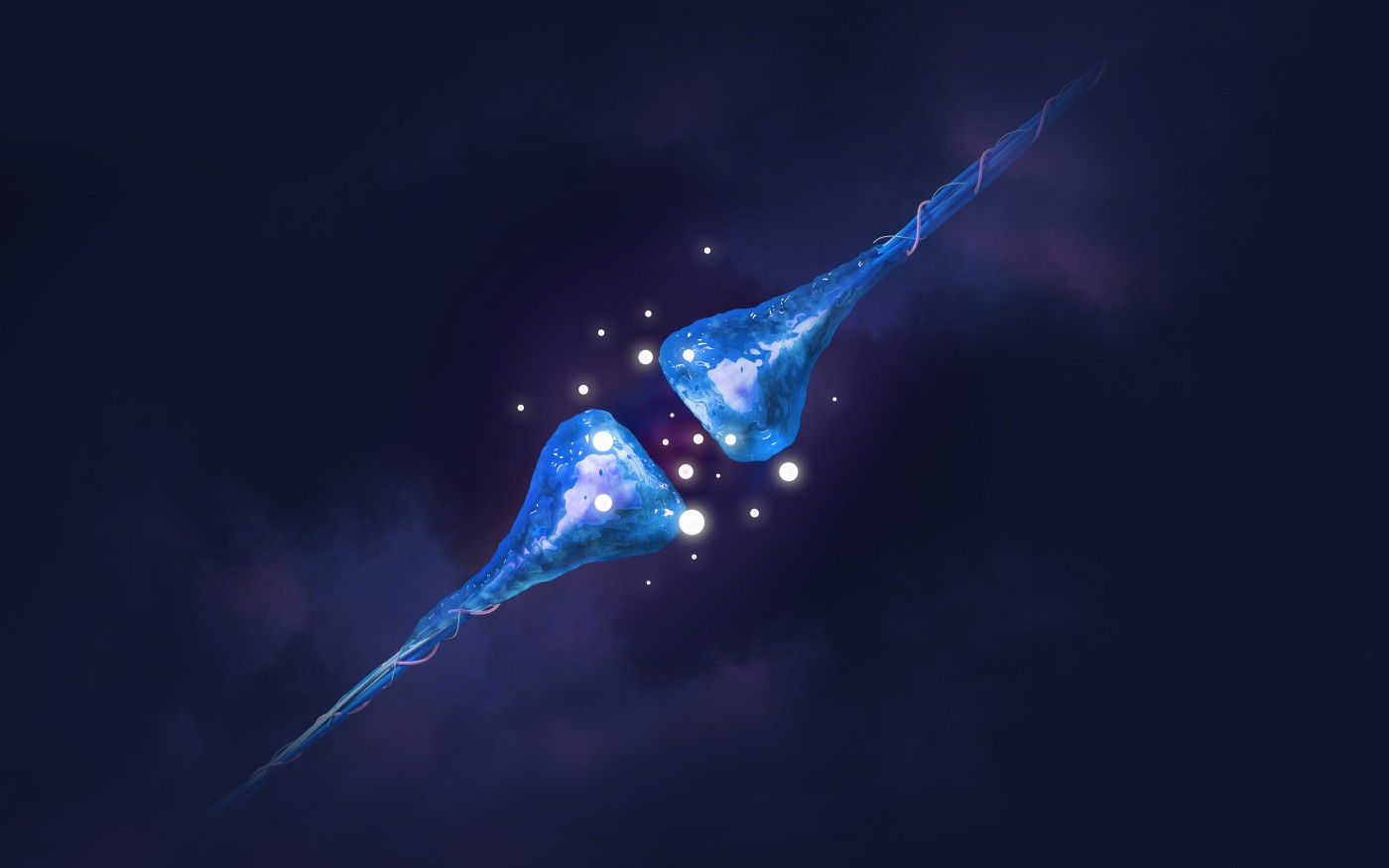
During development, synapses are eliminated by a system relying on brain immune molecules. A protein called C1q “tags” synapses that are to be disposed of, and microglial cells get rid of the synapses by simply eating them.
Researchers at Boston Children’s Hospital and Harvard Medical School have now used their extensive knowledge of developmental processes to understand changes also in the aging brain – obtaining new clues of how Alzheimer’s might arise. Their study, “Complement and microglia mediate early synapse loss in Alzheimer mouse models,” was recently published in the journal Science.
Such questions have remained largely unanswered in attempts to study the accumulation of amyloid-β in the brain of Alzheimer’s patients. The amounts of the protein deposits – amyloid plaques – show little agreement between the severity of symptoms, while loss of synapses correlate well with disease severity. So far, clinical trials targeting the accumulation of amyloid-β have also essentially failed, suggesting that the root of disease progression might be elsewhere.
“Synapse loss is a strong correlate of cognitive decline,” said Beth Stevens, assistant professor in the Department of Neurology at Boston Children’s, senior investigator of the study, in a press release. “We’re trying to go back to the very beginning and see how synapse loss starts.”
Led by Stevens, the research team studied different mouse models of Alzheimer’s disease, genetically engineered to produce excess amounts of amyloid-β. These mice are afflicted with cognitive problems as they age, and amyloid plaques litter their brains.
The team noticed that these mice also had a substantial loss of synapses and these animals had much higher levels of C1q in their brains long before plaques started accumulating. When researchers prevented C1q from functioning by using a C1q-blocking antibody, mice ended up with far more spared synapses. The same effect could be observed if they blocked another protein downstream of the C1q signaling pathway – C3.
This indicated that the process active during brain development was somehow turned back on in old age.
“Microglia and complement are already known to be involved in Alzheimer’s disease, but they have been largely regarded as a secondary event related to plaque-related neuroinflammation, a prominent feature in progressed stages of Alzheimer’s,” said Soyon Hong, Ph.D., of Boston Children’s F.M. Kirby Neurobiology Center and the study’s first author. “Our study challenges this view and provides evidence that complement and microglia are involved much earlier in the disease process, when synapses are already vulnerable, and could potentially be targeted to preserve synaptic health.”
The team also found that amyloid-β is indeed involved in Alzheimer’s pathology, although in a different way than previously suggested. When they injected a form of the amyloid-β protein known to form plaques into the brains of both normal mice and mice lacking C1q, normal mice lost a host of synapses. In contrast, the mutant mice were largely unaffected.
This indicates that amyloid-β and C1q together activates an immune response, involving the protein C3 and microglia, leading to the clearance of synaptic connections.
The work provides a totally new view of immune processes in Alzheimer’s, previously believed to be a reaction to the accumulation of plaques. While suggesting that the immune processes that might be at the root of the disease are still considered controversial, a human version of the antibody against C1q is currently being developed by Annexon Biosciences in San Francisco. Once the drug reaches clinical trials, the theory will undoubtedly be put to test.
“One of the things this study highlights is the need to look for biomarkers for synapse loss and dysfunction,” Hong said. “As in cancer, if you treat people at a later stage of Alzheimer’s, it may already be too late.”






