Origins of Alzheimer’s Traced to Basal Brain Region in Study That Challenges Current Beliefs
Written by |
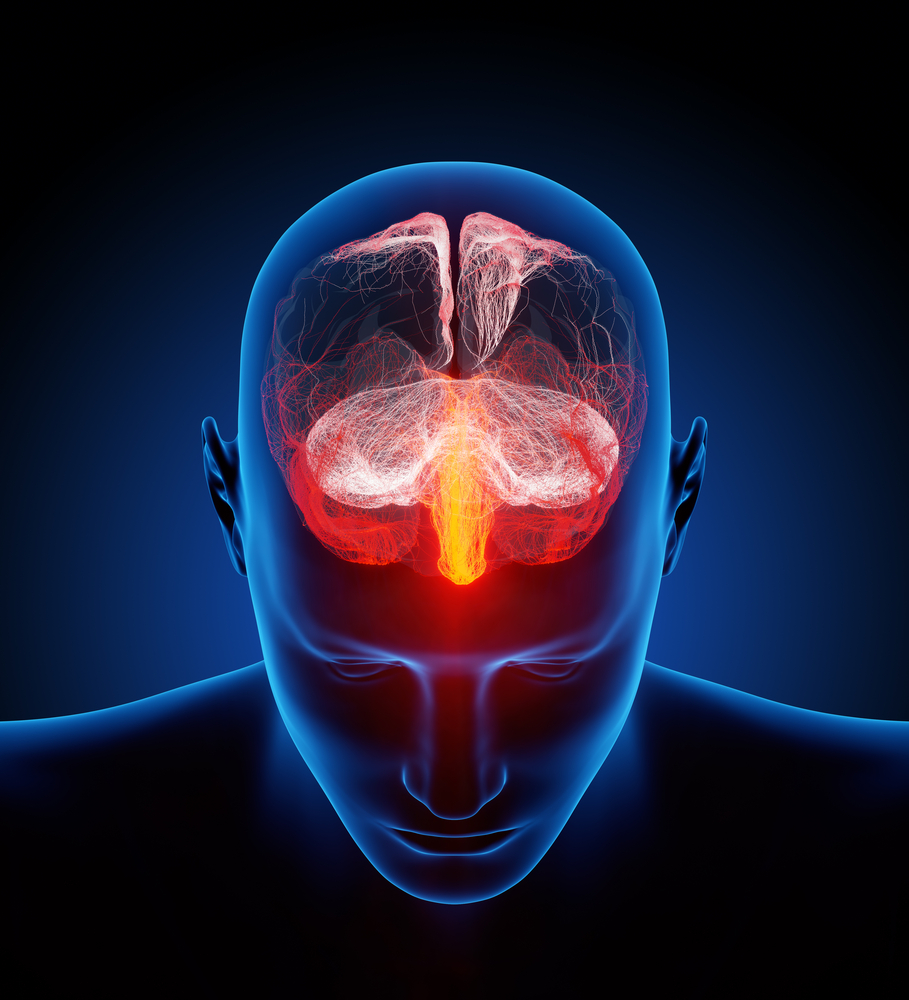
Alzheimer’s disease starts with neurodegenerative changes in basal brain structures, and spreads to more superficial layers as the disease progresses, new research reports — a finding that challenges the widely held view that the disease originates in the brain’s cortex.
The findings, reported in the study, “Basal forebrain degeneration precedes and predicts the cortical spread of Alzheimer’s Pathology,” which recently appeared in the journal Nature Communications, may allow researchers to develop treatments targeting events earlier in the disease than was previously possible, in attempts to stop it from progressing.
Investigations of brains of early Alzheimer’s patients have researchers arguing about the origin of the disease. Early on, neurodegeneration is present in two areas, called the basal forebrain and the entorhinal cortex. But so far, no one has been able to prove if neurons in one of these areas start dying before the other, or if the changes happen simultaneously in both regions.
Researchers from Cornell University in New York and the University of Cambridge in the U.K. analyzed brain imaging data from the Alzheimer’s Disease Neuroimaging Initiative database.
The database holds information on both cognitively healthy older adults, and those with various degrees of memory problems. One group of participants had diagnosed Alzheimer’s disease, while another had mild cognitive impairment. Of the people with only minor memory problems, some progressed to Alzheimer’s during a one-year follow-up.
All participants underwent high-resolution anatomical magnetic resonance imaging scans, measuring brain volumes, three times during a two-year period.
Analyzing the data, the research team noted that both Alzheimer’s patients and those with mild cognitive impairment had lost more tissue in both the basal forebrain and the entorhinal cortex than cognitively normal controls.
A more thorough examination revealed that the temporal lobes looked the same, irrespective of amyloid-beta levels in the cerebrospinal fluid of the participants. But seemingly healthy older adults who had high levels of amyloid in their spinal fluid had notable loss of tissue in the basal forebrain.
Researchers also concluded that neurodegeneration in this deeper brain structure predicted later tissue degeneration in the entorhinal cortex. In contrast, tissue loss in the entorhinal cortex could not predict degeneration in the basal forebrain.
“We’re hoping that this work pushes a bit of a reorganization of the field itself, to reappraise where the disease originates,” Nathan Spreng, a Cornell assistant professor of human development, said in a news release. “That could open up new avenues for intervention; certainly it would for detection.”
The team acknowledged that their findings are of limited impact for people at risk of developing Alzheimer’s today, as there is no way of stopping it, and may add to anxiety by making them more aware of their likelihood of developing the disease.
The value of the findings, instead, lie in informing future research that may find ways to stop the progression. “Our clarification of an earlier point of Alzheimer’s propagation is therefore of utmost importance for guiding endeavors to combat this devastating disease,” said Taylor Schmitz of the University of Cambridge’s Cognitive Brain Sciences Unit.





