Georgetown to Lead Phase 2 Study of Cancer Drug in Treating Alzheimer’s
Researchers at Georgetown University Medical Center (GUMC) are recruiting participants for a clinical trial to evaluate the cancer drug Tasigna (nilotinib) in people with mild to moderate Alzheimer’s disease (AD).
The randomized, double-blind, placebo-controlled Phase 2 clinical trial (NCT02947893) will evaluate how low doses of Tasigna impact safety, biomarkers, and clinical outcomes in 42 patients with mild to moderate AD.
Tasigna, a tyrosine kinase inhibitor, is used to treat a blood cancer called Philadelphia chromosome positive chronic myeloid leukemia (CML). The drug is usually administered when patients have failed to improve on other medications. It was approved by the U.S Food and Drug Administration (FDA) in 2010, and has been authorized in the European Union since 2007.
Safety, the trial’s primary focus, will be assessed based on the number of participants who experience adverse events or have abnormal laboratory values after 12 months of treatment.
The effect of the yearlong treatment is the secondary endpoint. Researchers will assess the drug’s ability to penetrate the blood-brain barrier, decrease beta-amyloid plaque in the brain, and reduce cerebrospinal fluid (CSF) markers of cell death.
The study, partially supported with $2.1 million from The Alzheimer’s Drug Discovery Foundation, is being conducted in partnership with MedStar Georgetown University Hospital.
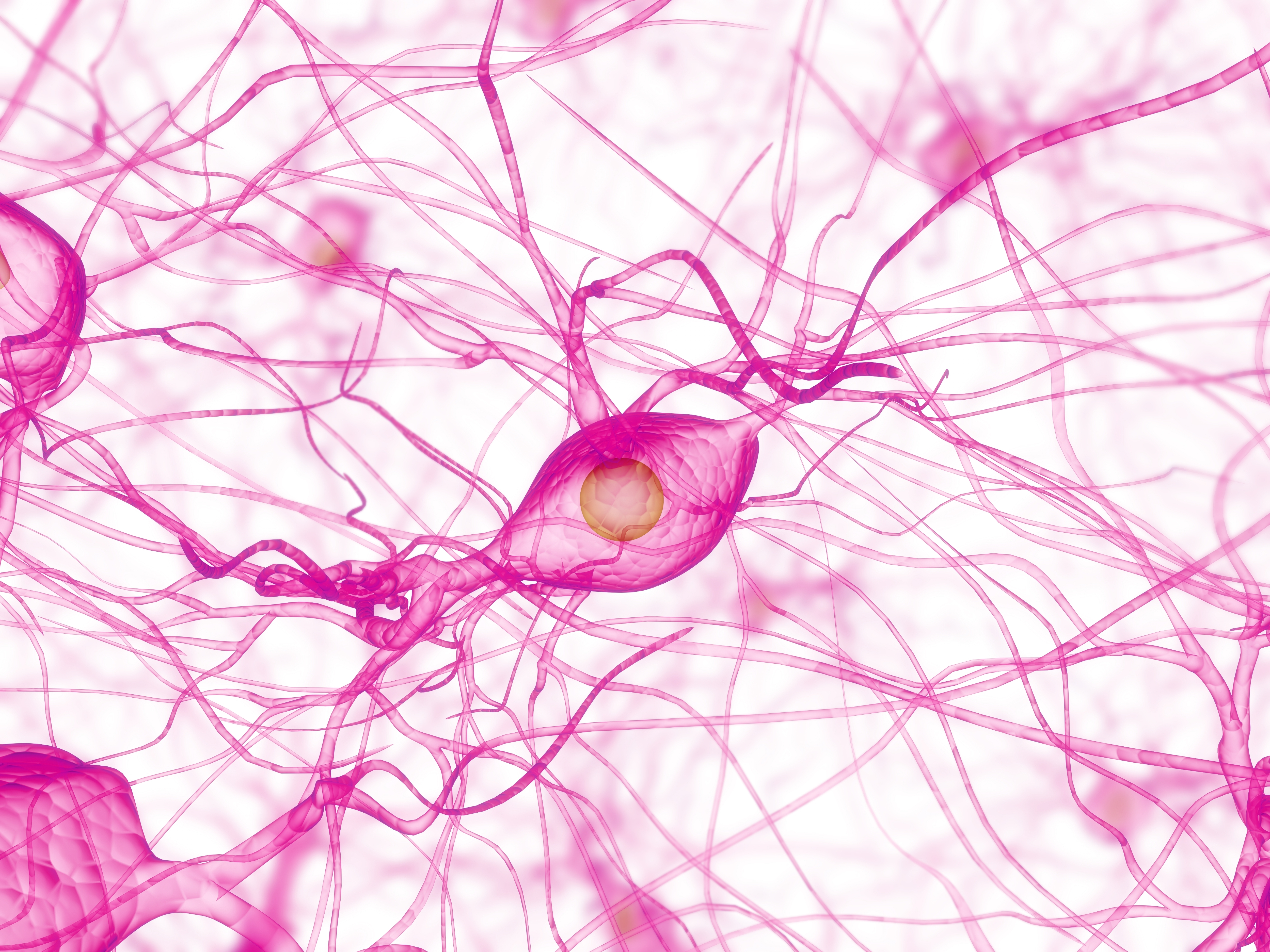
In laboratory and preclinical studies conducted at the Georgetown Translational Neurotherapeutics Program (TNP), Tasigna appeared to help clear accumulated beta-amyloid plaque and tau tangles in the brain; both are hallmarks of AD. In the studies, the drug seemed to penetrate the blood-brain barrier and turn on a process called autophagy to clear the tau, amyloid, and other toxic proteins.
Charbel Moussa, MB, PhD, who directs Georgetown’s Laboratory of Dementia and Parkinsonism, conducted the preclinical research that led to Tasigna being discovered to treat neurodegenerative diseases. Moussa and his colleagues reported in October 2015 that the drug could improve cognition and motor skills.
“In a 2015 proof of concept study at Georgetown, patients with Parkinson’s disease or dementia with Lewy bodies were treated with nilotinib. As my colleagues reported, those who completed the study had a reversal in disease progression, observed both clinically and in key biomarkers — the same biomarkers seen in Alzheimer’s,” Scott Turner, MD, PhD, medical co-director of the TNP, said in a news release. He will be the principal investigator for the study.
“But even before the Parkinson’s study, research in the laboratory strongly supported studying this drug in people with Alzheimer’s,” Turner said. “The promising results of the Parkinson’s study give an even stronger rationale.”
A lower dose of Tasigna will be used in the study than is usually administered to treat CML, Moussa said.
“When used in smaller doses once a day, as in this study, it appears nilotinib turns on autophagy for about four to eight hours — long enough to clean out the cells without causing cell death. Toxic proteins that build up again then appear to be cleared when the drug is given again the next day.”






