High Calcium Levels in Mitochondria Cause Neuronal Death in Alzheimer’s, Study Shows
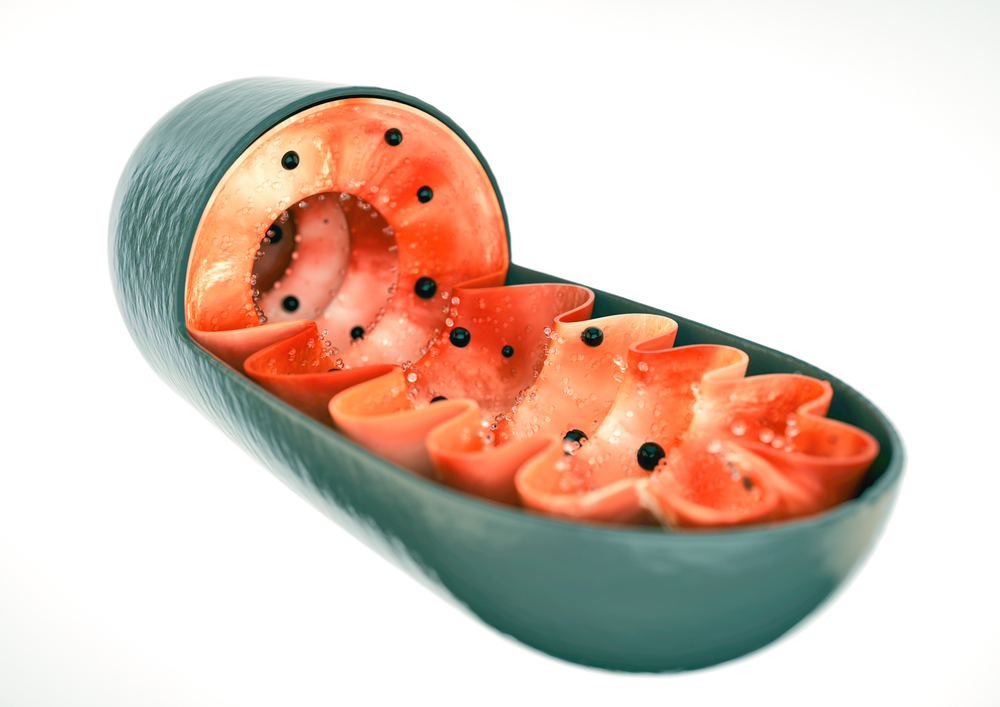
Abnormal levels of calcium in the mitochondria, the cell’s powerhouse, may lead to neuronal death in Alzheimer’s disease and dementia, according to researchers at Temple University’s Center for Translational Medicine.
Scientists presented their study, “Imbalance of calcium in a cell’s energy factory may drive Alzheimer’s disease,” at the 61st Meeting of the Biophysical Society, held Feb. 11-15 in New Orleans.
Calcium is a crucial signaling messenger in the brain, which is why its levels are tightly regulated within neurons. Previous studies have shown that calcium levels in the mitochondria control energy production, and that too much calcium may lead to neuronal death. But the specific relationship between mitochondrial calcium and cell death in Alzheimer’s remained elusive.
Using brain samples from Alzheimer’s patients, researchers observed very low levels of mitochondrial sodium/calcium exchanger, the protein that transports calcium out of the mitochondria in neurons. That deficiency means that calcium ions are trapped inside the mitochondria after entering this organelle, where they begin to accumulate.
The toxic increase in calcium inside the mitochondria disrupts the normal functioning of the mechanisms that produce energy, triggering excessive levels of oxidant molecules, which damage the mitochondria and neurons. Low levels of the transporter are therefore linked to increased mitochondrial impairment and cell death, contributing to neuronal loss in Alzheimer’s.
In mice models of this disease, researchers found that before the onset of symptoms, the expression levels of the gene encoding the mitochondrial sodium/calcium exchanger also drop, which may be the start of disease progression. However, when researchers enhanced the expression of this gene in diseased mice, mitochondrial activity recovered and the affected neurons became similar to healthy neurons.
“No one’s ever looked at this before using these model systems,” the study’s senior researcher, John Elrod, said in a news release. “It’s possible that alterations in mitochondrial calcium exchange may be driving the disease process.”
The team now plans to investigate whether promoting the expression of a transporter gene can potentially reverse progression of Alzheimer’s in mice. If their hypothesis is correct, the transporter gene and the associated signaling mechanism may become valuable targets for novel therapies aimed at improving mitochondrial function in Alzheimer’s.
“Our hope is that if we can change either the expression level or the activity of this exchanger, it could be a viable therapy to use early on to perhaps impede Alzheimer’s disease development. That’s the home run,” Elrod said, though he added: “We’re not even close to that.”






