Vanderbilt Researchers’ Potential Alzheimer’s Therapy Being Tested in Phase 1 Study
Written by |
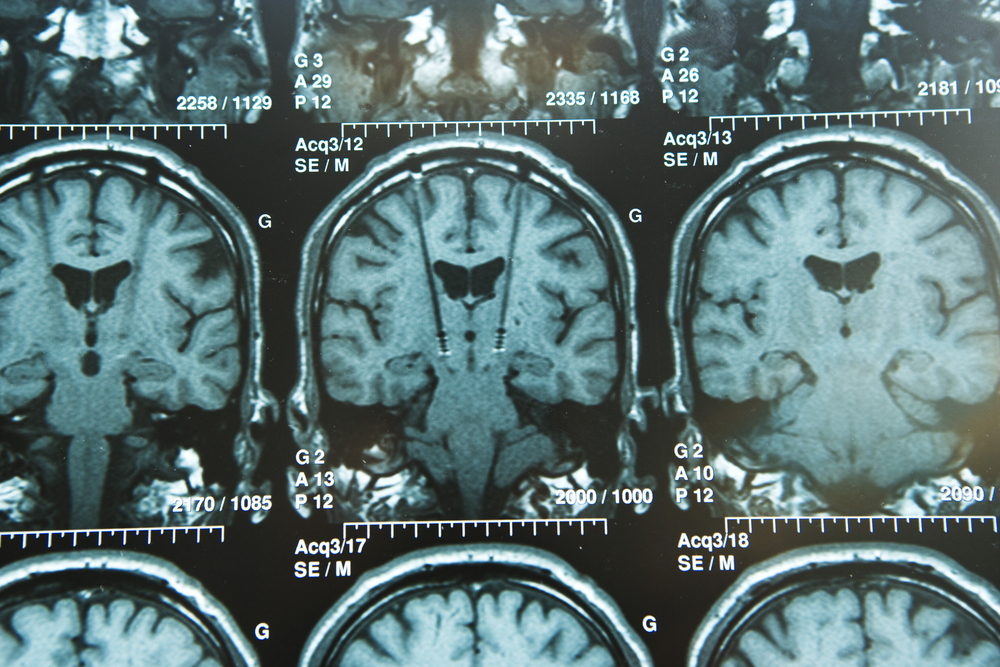
Vanderbilt University researchers have developed a potential therapy for Alzheimer’s disease (AD) that has shown promising results in brain health.
The investigative treatment, a molecule called VU319, is expected to fill a long-needed gap for Alzheimer’s patients by improving memory, attention, and brain functioning. The U.S. Food and Drug Administration (FDA) has cleared the drug to move into human clinical trials to determine the proper dose and safety profile.
VU319 is currently being tested in healthy human volunteers. The first patient was dosed on July 29 in a first-in-human Phase 1 clinical trial at the Vanderbilt Institute for Clinical and Translational Research.
If it passes the Phase 1 study in healthy people, VU319’s abilty to improve cognitive function will be tested in patients with Alzheimer’s disease and other brain disorders.
VU319 was developed by a team of scientists at the Vanderbilt Center for Neuroscience Drug Discovery led by center director P. Jeffrey Conn and Craig W. Lindsley, co-director of the center.
“This new small-molecule approach to potentially treating Alzheimer’s disease represents an exciting advance from currently available therapies,” Dr. Paul Newhouse, director of the Vanderbilt Center for Cognitive Medicine and leader of the study, said in a press release.
Newhouse and his team spent three years testing VU319 in animals after developing it from a molecule, also discovered at Vanderbilt.
The fact that the new drug went from “bench to bedside” — an expression used by Newhouse — is an important part of the discovery for the researchers, who believe this may be the first time an “academic drug discovery group moved a molecule designed to treat a chronic brain disorder from laboratory bench to early clinical trials without a pharmaceutical company partner,” according to the press release.
VU319 is a positive allosteric modulator (PAM) because it increases the activity of a receptor in the brain, sort of like a light dimmer switch. The target is the M1 muscarinic acetylcholine receptors, which are located on neurons activated by the neurotransmitter acetylcholine.
In related news, Loyola Medicine is still recruiting patients for its landmark $100 million study called “Imaging Dementia – Evidence for Amyloid Scanning (IDEAS)” to evaluate the effectiveness of using positron emission tomography (PET) scans to detect Alzheimer’s.
The IDEAS (NCT02420756) study will enroll 18,488 Medicare beneficiaries who have been diagnosed with mild cognitive impairment or dementia of an unknown cause.
There are many trial sites where people can participate (full list here) and you can use the IDEAS study website site locator to find the one closest to your home.
For more detailed information about enrollment and eligibility, contact Cynthia Olson at [email protected] or Leslie Sears at [email protected].





