Dysregulation of Iron Could Play a Central Role in Development of Early Onset Alzheimer’s
Iron dysregulation in the brains of patients with early onset of Alzheimer’s disease (EOfAD) plays a central role in disease development and progression, according to a new theory.
The study, “Dysregulation of Neuronal Iron Homeostasis as an Alternative Unifying Effect of Mutations Causing Familial Alzheimer’s Disease,” was published in the journal Frontiers in Neuroscience.
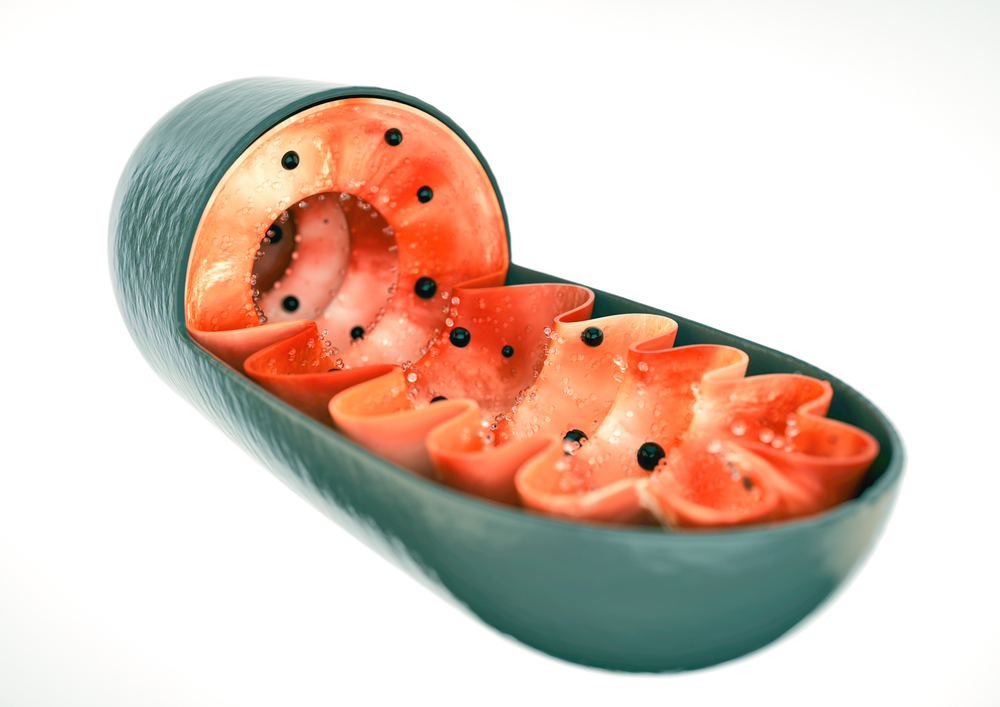
Iron, the most abundant transition metal in the human body, plays a key role in the production of energy by the mitochondria — the compartment of the cell responsible for meeting all of the cell’s energy needs.
A charged version of iron, called Fe2+, is the required form for aerobic respiration (the most efficient way in which the mitochondria produce energy). It is extremely important to manage levels of Fe2+ as imbalances can lead to oxidative stress and development of inflammation.
Several lines of evidence suggest that iron levels are imbalanced in patients with Alzheimer’s disease. First, these patients have significantly higher levels of protein aggregates called amyloid-β (Aβ) plaques, which are highly enriched with heme, a component of which is iron.
Next, levels of ferritin (the iron storage complex) in cerebrospinal fluid (CSF) is significantly higher in patients who have a particular variant of the gene APOE that is associated with late-onset Alzheimer’s disease (LOsAD). Additionally, ferritin levels in the CSF also are predictive of conversion from mild cognitive impairment (MCI) to Alzheimer’s disease.
Furthermore, levels of ferritin in plasma (a component of blood) strongly correlate with Aβ levels in the neocortex (area of the brain involved in higher-order brain functions). In fact, assessing plasma ferritin levels can help identify which patients are at a high risk for developing Alzheimer’s disease.
Early-onset of Alzheimer’s disease is caused mainly by mutations in three genes, called PSEN1, PSEN2, and APP. These genes are mediators of iron. “The genes mutated in inherited Alzheimer’s disease seem likely to affect how iron enters neurons, how it is recycled within neurons, and how it is exported from neurons,” study author Michael Lardelli, associate professor at the University of Adelaide, said in a press release.
In fact, APP’s role in iron export is so important that its expression is actually indirectly regulated by the presence of iron. Additionally, PSEN genes play a role in the proper functioning of cellular compartments called endosomes/lysosomes, which are the major routes through which iron enters cells.
“Since neurons have such huge energy needs, disturbing the way they handle iron can have serious, long-term consequences,” Lardelli adds.
While the reason behind the development of Alzheimer’s disease is not known, most researchers ascribe to the amyloid hypothesis. “For 20 years most scientists have believed that a small protein fragment, amyloid beta, causes Alzheimer’s disease,” says Lardelli.
However, he said, “Clearing out amyloid beta from the brains of people who are developing Alzheimer’s disease can slow their rate of cognitive decline. But, so far, nothing has been able to stop the relentless progression of the disease.”
Researchers now suggest another hypothesis in which the aging vasculature, hypoxia (low levels of oxygen), iron, and energy production contribute to the development of EOfAD.
Essentially, high levels of hypoxia, which is characteristic of normal aging in the brain, skews metabolism toward glycolysis (an inefficient method of obtaining energy).
However, the brain cannot continuously rely on glycolysis, so it reverts to a hypometabolic (low metabolism), dysfunctional state.
Researchers suggest that EOfAD mutation-associated dysregulation of Fe2+ causes the brain to revert to glycolysis earlier, which otherwise would be used to cope with the hypoxia caused by natural aging.
Then, a trigger, such as an infection or heart failure, leads the brain over a “stress threshold” — causing high levels of inflammation and hypometabolism that characterize AD.
“This stress threshold is exceeded sooner in the pre-stressed brains of EOfAD mutation carriers than in non-carriers, leading to an earlier onset of Alzheimer’s disease,” the authors explained.
“[W]e suggest that a concentration of effort in this area [iron imbalance] will give us valuable insights into the pathogenesis of Alzheimer’s disease,” they concluded.






