Mitochondrial Gene May Protect Against Alzheimer’s, Other Aging-related Diseases, Study Reports
A previously unknown genetic risk factor for Alzheimer’s disease and related dementias has been uncovered.
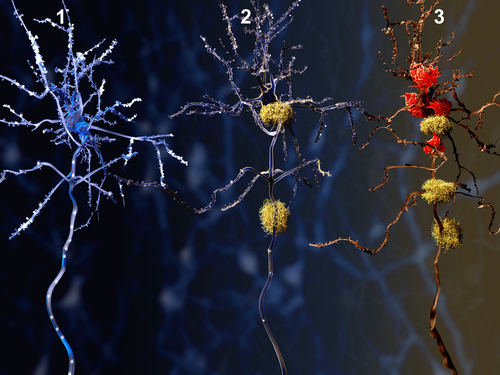
The culprit, known as humanin, is a neuroprotective factor known to decrease with age. It can protect brain cells from accumulating amyloid beta — a key player in the development of Alzheimer’s disease.
“Because of the beneficial effects of humanin, a decrease in circulating levels could lead to an increase in several different diseases of aging, particularly in dementia,” Pinchas Cohen, MD, dean of the USC Leonard Davis School of Gerontology and one of the scientists who discovered humanin 15 years ago, said in a press release.
The study, “Humanin Prevents Age-Related Cognitive Decline in Mice and is Associated with Improved Cognitive Age in Humans,” was published in the journal Scientific Reports.
Humanin is a naturally occurring peptide, or small protein, produced by mitochondria, which are the small cellular organelles that provide energy to cells. It is specifically encoded within the mitochondrial genome, which is independent and differs from the nuclear genome,which is present in the nucleus of each cell and contains most of our genetic information.
Humanin has been shown to be neuroprotective in multiple studies, both in cellular and animal models. The importance of the mitochondria in the development of Alzheimer’s disease is becoming more apparent, and evidence suggests that humanin can protect against amyloid-beta toxicity as well as other familial forms of Alzheimer’s disease and prevent memory deficits.
After finding that humanin was able to decrease age-related cognitive decline in a mouse model of aging — by decreasing inflammation both in the brain and throughout the body — researchers hypothesized that differences in circulating humanin levels could partially account for the known ethnic disparities in neurocognitive diseases between Caucasian-Americans and African-Americans. The latter is known to be more affected by Alzheimer’s disease and other aging-related diseases.
The team used samples from the B-Vitamin Atherosclerosis Intervention Trial (BVAIT) (NCT00114400), from which they selected 71 African-Americans and 75 Caucasian-Americans matched by gender, age, and randomized treatment.
“This group was made up of male and female patients at least 40 years old with no signs or symptoms of cardiovascular disease,” the researchers wrote.
Results showed a significant difference between the two groups, with African-Americans having a mean circulating humanin level 20% lower than Caucasian-Americans.
“We have now discovered a novel underlying biological factor that may be contributing to this health disparity,” said Kelvin Yen, PhD, a research assistant professor of gerontology at the USC Leonard Davis School who led the study.
Researchers screened the entire mitochondrial genome looking for common genetic variations, known as single nucleotide polymorphisms, or SNPs, that could explain the changes in humanin levels. SNPs are the most common type of genetic variation in people, with each SNP representing an alteration in a single DNA building block, or nucleotide.
Through this analysis, they found an SNP called rs2854128 that was associated with a 14% decrease in circulating humanin levels.
“Both self-reported race and the presence of the rs2854128 SNP independently and additively contributed to predicting humanin levels,” the researchers wrote.
The team then examined the effects of this specific SNP in a separate group of participants from the Health and Retirement Study, a longitudinal study of approximately 20,000 individuals older than 50 in the U.S. More than 12,500 individuals consented to DNA analysis.
Results revealed that the original gene without the SNP is found in 42% of Caucasian-Americans and in a much lower percentage of African-Americans (1.7%) and Hispanics (6%). Importantly, low levels of humanin were also associated with accelerated cognitive aging.
“The role of humanin in health disparities is a novel concept that further implicates the mitochondria in the biological basis of health disparities,” the authors wrote.
“This SNP is associated with accelerated cognitive aging, supporting the concept that humanin is an important factor in cognitive aging,” they concluded.






