$47M Federal Grant Adds Brain Imaging to Pivotal Lifestyle Interventions Study
The University of California, Berkeley (UC Berkeley) will receive an expected $47 million in a federal grant that will add advanced brain imaging to a pivotal study to determine whether lifestyle modifications can protect memory in those at risk of developing dementia.
With the five-year grant from the U.S. National Institute on Aging (NIA), the university will conduct the first large-scale clinical investigation (NCT03688126) — currently recruiting participants — examining how affordable and accessible lifestyle changes affect biomarkers of Alzheimer’s disease and dementia. The study will focus on changes such as exercise, diet, cognitive stimulation and health coaching. More information on how to participate can be found here.
The award total is pending funding availability. The NIA is part of the National Institutes of Health. The multisite randomized study was originally funded with $35 million from the Alzheimer’s Association.
If successful, the “U.S. Study to Protect Brain Health Through Lifestyle Intervention to Reduce Risk (U.S. POINTER)” is expected to affect public policy regarding the standard of care for a growing patient population. According to the non-profit, the number of U.S. residents living with Alzheimer’s disease — currently 5.8 million — could nearly triple to 13.8 million by 2050.
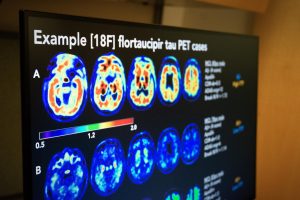
As part of the new Neuroimaging Ancillary Study, funded by the National Institute on Aging, U.S. POINTER study participants will be assessed with PET imaging and MRI scans to measure the biological impact of lifestyle changes on brain health.
(Photo by Malachi Tran, University of California, Berkeley)
The grant will support the U.S. POINTER Neuroimaging Ancillary Study, which will use advanced brain imaging to measure the biological impact of lifestyle changes on brain health. Researchers will assess overall and regional brain shape, size, and blood flow, and risk for heart and small-vessel disease. Imaging techniques will include amyloid-beta positron emission tomography (PET), tau PET, and magnetic resonance imaging (MRI) scans. Neuronal aggregates, or clumps of abnormal forms of beta-amyloid and tau proteins are considered disease biomarkers.
“A healthy diet and lifestyle are generally recognized as good for health, but U.S. POINTER is the first large randomized controlled trial to look at whether lifestyle changes actually influence Alzheimer’s disease-related brain changes,” Susan Landau, a UC Berkeley research neuroscientist and principal investigator of the add-on study, said a press release. “Lifestyle modification is a non-drug option that is accessible to people and may reduce the risk of developing Alzheimer’s.”
U.S. POINTER will test whether lifestyle interventions combining healthy nutrition, physical activity, social and intellectual challenge, and increased monitoring of vascular and metabolic conditions can protect cognitive function in adults ages 60 to 79 who are at risk for cognitive decline. It follows recommendations from the 2018 NIH Alzheimer’s Research Summit that encouraged studies of lifestyle interventions to prevent Alzheimer’s and other dementia.
“This groundbreaking project is an unparalleled examination of how lifestyle ‘therapies’ may change our brain in ways that are related to Alzheimer’s disease, vascular dementia and overall brain health,” said Maria C. Carillo, PhD, chief science officer of the Alzheimer’s Association. “The addition of brain imaging is an important component that could provide the roadmap for brain health to reduce the risk of dementia before symptoms have a chance to appear.”
A key trial feature is its recruitment approach, which seeks to include a geographically, and racially and ethnically diverse population. This will help ensure the intervention can be applied to a large proportion of older adults. The study will take place at four sites: Winston-Salem, N.C.; Houston; Davis, Calif.; and Chicago. Another site will be announced later this year.
To measure the buildup of amyloid and tau, up to 1,250 of 2,000 study participants will undergo PET imaging at the study’s start and at the two-year mark. To measure brain region size, identify lesions related to vascular changes, and observe blood flow changes, patients will undergo a baseline MRI followed by another one at one and two years.
“Brain markers of dementia, when measured at the beginning of the study, may predict who will respond best to the interventions, which could inform future precision medicine approaches to healthcare,” Landau said.
The study was prompted by the success of the “Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER)” investigation (NCT01041989). Those findings showed that in at-risk adults, lifestyle changes improved cognitive function by 25% relative to adults randomly selected to receive health education. Multiple other studies based on that model are being coordinated through an interdisciplinary global network called World Wide FINGERS.






