Understanding Protein Aggregation May Aid Quest for Better Alzheimer’s Treatments
Better understanding the mathematics behind how protein clumps form — and how therapies interfere with this process — may improve treatment strategies for Alzheimer’s, and other diseases, new research suggests.
The study, “Optimal control strategies for inhibition of protein aggregation,” was published in PNAS.
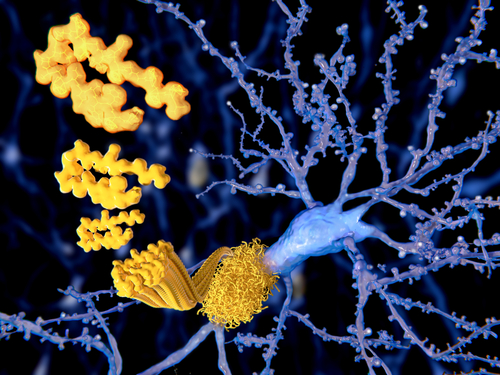
Protein aggregation is the term for when proteins — usually misfolded ones — form clumps. This process is thought to play a role in a number of diseases, particularly Alzheimer’s and Parkinson’s. But even though “proteins forming clumps” sounds like a simple process, it involves a number of steps.
First, there is primary nucleation, in which a few individual proteins come together to form a fibril — basically a little strand of proteins linked together. The fibril then grows longer as more proteins are added. The process of fibril formation and growth can take a long time (years or even decades), which may explain why Alzheimer’s typically is seen only in older people.
Once the fibrils reach a critical mass, secondary nucleation begins. Once there are enough clumps, more clumps start forming faster and faster, growing at an exponential rate.
The researchers behind the new study used this understanding of the physics of protein aggregation in combination with control theory (a framework for understanding systems that are constantly changing) to make predictions about how different treatments would affect protein aggregation and, by extension, disease progression.
“By combining well-known concepts from two different fields, the kinetics of protein aggregation, and optimal control theory, we linked molecular-scale phenomena to macroscale strategies with relevance for a real, practical problem,” L Mahadevan, PhD, a professor at Harvard and co-author of the study, said in a press release.
The investigators then checked their predictions against previously published data on protein aggregation-blocking treatments in the worm model C. elegans.
In simplest terms, the researchers found that the aggregation-blocking power of a given therapy depended on when it was administered combined with whether it blocked primary or secondary nucleation.
For example, the cancer drug bexarotene selectively inhibits primary nucleation; as such, treatment with bexarotene was effective in the early stages of disease, but not the latter stages. In contrast, DesAb29-35, an antibody designed to block secondary nucleation, was more effective in latter, but not earlier, disease stages. Both these compounds inhibit the aggregation of amyloid-beta — the main component of senile plaques in Alzheimer’s and of normal aging — but at different steps.
“Our research highlights the importance of understanding the relationship between the chemical kinetics of protein misfolding, the mechanisms by which drugs inhibit protein aggregation, and the timing of their administration,” said Mahadevan. “This understanding could have important implications for intervention protocols to prevent pathological protein aggregation.”
Thomas C. T. Michaels, PhD, another study co-author who is a postdoctoral fellow at Harvard, added that these findings “will allow people to test the efficacy of different compounds against aggregation under optimal conditions at the drug discovery and drug screening level. From these optimal conditions, one could then extrapolate optimal conditions for a [clinical] trial. So, in this sense, our work could help seed potential trials.”






