In Alzheimer’s Patients, Blood Flow to Brain Appears Hampered by Plaques
Written by |
A recent study suggests that amyloid beta plaques may alter normal blood flow to brain tissue and contribute to development of Alzheimer’s disease. The paper, published in the journal Brain, is entitled “Vascular amyloidosis impairs the gliovascular unit in a mouse model of Alzheimer’s disease.”
Alzheimer’s involves numerous complicated processes, and the causes and mechanisms of its development are not yet clearly defined. A number of studies have highlighted the presence of abnormal levels of extracellular amyloid beta plaque deposits in the brain tissue of Alzheimer’s patients, but how these deposited plaques affect brain activity is still debated.
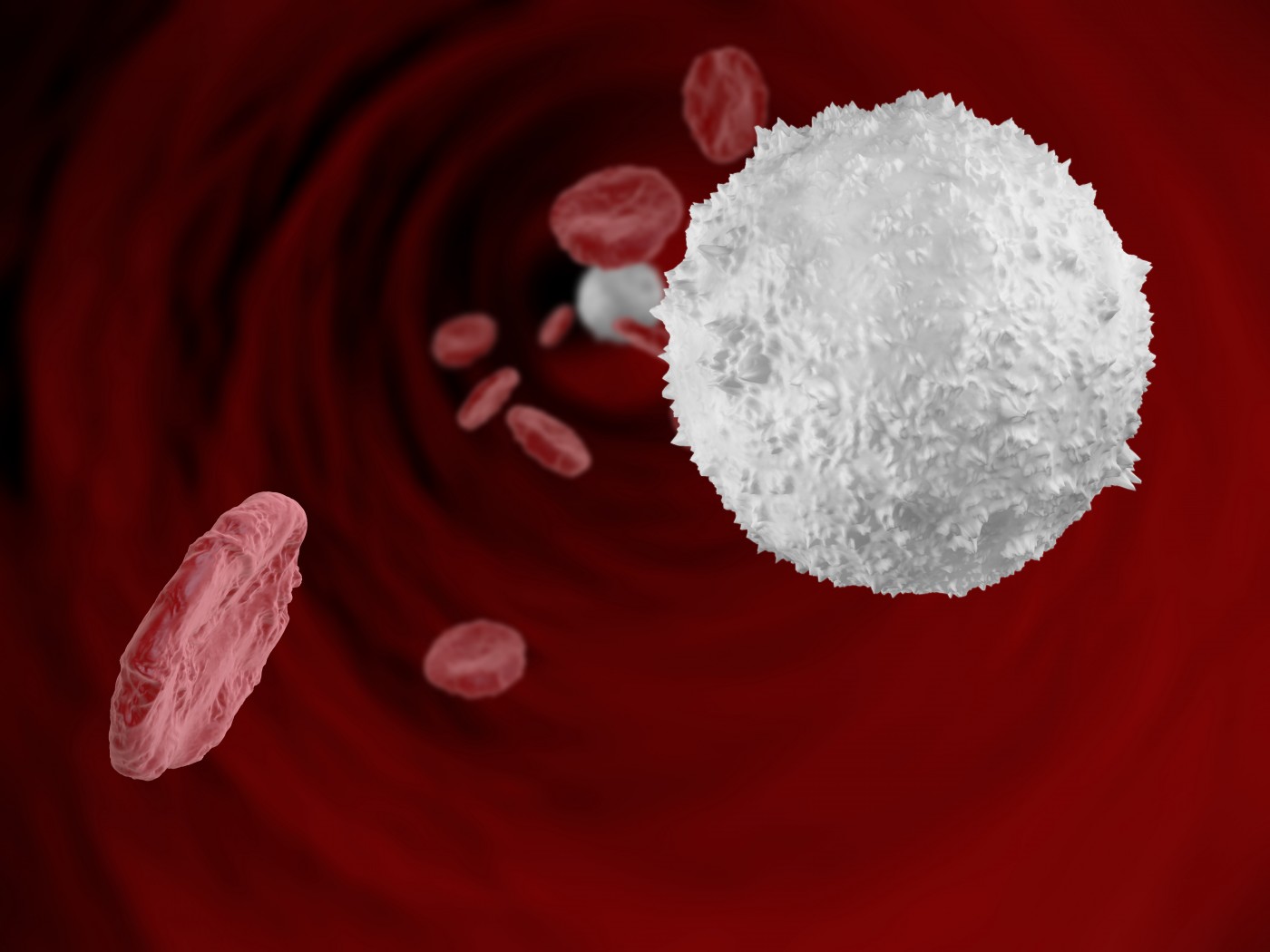
Nerve cells extract energy from glucose sugar transported through the blood stream. In this process, cells called astrocytes are involved in the regulation of blood flow through vessels by increasing and decreasing their diameters according to signals received from a mediating species named astrocytic endfeet. A study published in 2014 showed that in brain tumors, malignant astrocytes may travel through blood vessels to interfere with function of astrocytic endfeet in regulating blood flow.
In this study, the researchers investigated whether amyloid beta plaques similarly interfere with the role of astrocytic endfeet in regulating blood flow. They used advanced laser-scanning microscopes to visualize deep into a living brain to form three-dimensional, volumetric images of brain morphology.
“In a live animal model of Alzheimer’s disease, we then activated the vascular smooth muscle cells with a pulsed laser, allowing us to mimic neuron-induced astrocyte-vascular signaling. In locations where no vascular amyloid was present, we saw a very dramatic and robust vessel response; however, on blood vessels that were surrounded by plaque, we saw a much diminished response,” said Ian Kimbrough, a graduate research assistant in Neurobiology and a collaborator on the original brain tumor study, in a new release.
“Using this 3-D model, which we can rotate and manipulate, we can see the exact spatial relationship between the vasculature, the astrocytic endfeet and the vascular amyloid. This allows us to analyze how these elements interplay in a normal, healthy brain compared to an Alzheimer’s disease brain,” Kimbrough added.
The results suggest that vascular amyloid plaque does in fact interfere with function of astrocytic endfeet in regulating blood vessels. The accumulated amyloid plaque forms rings around the vessels and deposits a rigid exoskeleton, restricting their ability to change in diameter when increased blood flow is requested by neurons. “The vessel has to be able to expand and contract, to dilate and constrict, if it’s going to regulate blood flow. If they have become rigid like a pipe, instead of having a flexible wall that can go back and forth, then they cannot do their job of regulating blood flow to the brain properly,” said Erik Roberson, MD, PhD, associate professor in the UAB Department of Neurology.
Overall, these findings demonstrate that amyloid beta plaque could account for the decrease in cerebral blood flow in patients with Alzheimer’s disease. “This was among the first studies to really attempt to understand the relationship between vascular amyloid and blood flow in the brain. For the first time, using the amazing technology at our disposal, we can see what is happening in the vessel walls in real time, to better understand how the presence of vascular amyloid effects the function of that vessel,” Dr. Roberson added.





