Australian Scientists Make Alzheimer’s Treatment Breakthrough Using Ultrasound Technology
Written by |
Scientists at Australia’s University of Queensland have found that non-invasive ultrasound technology can be used to break up neurotoxic amyloid plaques that cause memory loss and cognitive decline in persons afflicted with Alzheimer’s Disease (AD), which affects more than two-thirds of dementia patients.
The discovery is elucidated in a paper published in the March 11 edition of the journal Science Translational Medicine entitled “Scanning ultrasound removes amyloid- and restores memory in an Alzheimer’s disease mouse model“ (Sci Transl Med 11 March 2015: Vol. 7, Issue 278, p. 278ra33 DOI: 10.1126/scitranslmed.aaa2512) coauthored by PhD student Gerhard Leinenga and Professor Jurgen Götz of the Queensland Brain Institute’s Clem Jones Centre for Ageing Dementia Research, at the University of Queensland St. Lucia Campus in Brisbane, Queensland, Australia, who note that Amyloid- (A) peptide has been implicated in Alzheimer’s disease (AD) pathogenesis. The researchers present a nonpharmacological approach for removing A and restoring memory function in a mouse model of AD in which A is deposited in the brain. They discovered that repeated scanning ultrasound (SUS) treatments of the mouse brain can remove A without resort to any additional therapeutic agents such as anti-A antibody.
Dr. Götz and Mr. Leinenga employed spinning disk confocal microscopy and high-resolution three-dimensional reconstruction to reveal extensive internalization of A into the lysosomes of activated microglia in mouse brains subjected to SUS, and observed no concomitant increase in the number of microglia. They discovered that plaque burden was reduced in SUS-treated AD mice compared to sham-treated animals, with plaque-clearing observed in 75 percent of SUS-treated mice.
The coauthors report that treated AD mice also displayed improved performance on three memory tasks: the Y-maze, the novel object recognition test, and the active place avoidance task, concluding that their findings suggest repeated SUS can be useful for removing A in the mouse brain without causing overt damage, and should be explored further as a noninvasive method with therapeutic potential in AD.
 Commenting on the researchers findings at a press conference last week during a visit to UQs Queensland Brain Institute, Queensland Premier Annastacia Palaszczuk noted that “The Governments $9 million investment into this technology was to drive discoveries into clinics, and todays announcement indicates that together with the Queensland Brain Institute, it was a worthwhile investment. I want my Government to encourage more of this type of innovative research. Our Advance Queensland initiative aims to increase research and discoveries like this and to put this state’s research at the forefront internationally by supporting local researchers and helping to keep them in Queensland.”
Commenting on the researchers findings at a press conference last week during a visit to UQs Queensland Brain Institute, Queensland Premier Annastacia Palaszczuk noted that “The Governments $9 million investment into this technology was to drive discoveries into clinics, and todays announcement indicates that together with the Queensland Brain Institute, it was a worthwhile investment. I want my Government to encourage more of this type of innovative research. Our Advance Queensland initiative aims to increase research and discoveries like this and to put this state’s research at the forefront internationally by supporting local researchers and helping to keep them in Queensland.”
“These exciting findings will hopefully be of benefit to all Australians in the future,” the Premier concluded.
 QBI Founding Director Professor Perry Bartlett noted that the discovery is a result of game-changing work performed at the Queensland Brain Institutes Clem Jones Centre for Ageing Dementia Research (CJCADR) that was enabled by State and Federal Government funding and philanthropic support spearheaded by the Clem Jones Foundation.
QBI Founding Director Professor Perry Bartlett noted that the discovery is a result of game-changing work performed at the Queensland Brain Institutes Clem Jones Centre for Ageing Dementia Research (CJCADR) that was enabled by State and Federal Government funding and philanthropic support spearheaded by the Clem Jones Foundation.
“The farsighted investment of government and philanthropic partners has allowed us to build the research excellence and capacity required to make major discoveries such as this,” Professor Bartlett said, adding “I believe the work opens up an entirely novel avenue for future therapeutic treatment.”
Professor Bartlett and his own research team have played a significant role in debunking the dogma that the brain cannot produce new neurons. His group is dedicated to better understanding of mechanisms that drive continuous new neuron production in the adult brain sector called the hippocampus. This process, neurogenesis, slows as the body ages, with the resulting neuron deficit having been associated with cognitive function disorders.
Professor Bartlett’s laboratory has identified several regulatory factors, including Wnt3a and prolactin, which control neurogenesis in the hippocampus — discoveries that open the prospect of developing therapeutics to reverse cognitive decline in ageing brains.
Professor Jurgen Götz who is inaugural Director of the Clem Jones Centre for Ageing Dementia Research, told reporters that the new treatment method could revolutionizeAlzheimer’s treatment by restoring memory.
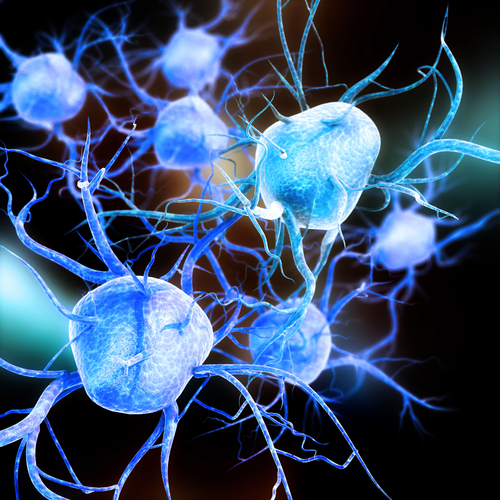
“We’re extremely excited by this innovation of treating Alzheimer’s without using drug therapeutics,” Professor Götz noted. “The ultrasound waves oscillate tremendously quickly, activating microglial cells that digest and remove the amyloid plaques that destroy brain synapses. The word breakthrough is often mis-used, but in this case I think this really does fundamentally change our understanding of how to treat this disease, and I foresee a great future for this approach.”
 Professor Götz’s own major research interest is focused on dissecting pathomechanisms in neurodegenerative diseases such as Alzheimer’s and frontotemporal dementia (FTD), and exploiting molecular insight revealed toward development of therapies. He and his team use genetically modified model organisms and eemploynovel gene editing methods in order to improve these models. Key molecules of interest are tau, kinases such as Fyn and Pyk2, and amyloid-beta, and therapeutic strategies include small molecules, antibodies and peptides. The laboratory also strives to understand selective vulnerability in human neurodegenerative diseases, and to improve methods used to deliver therapeutic agents past the blood-brain barrier.
Professor Götz’s own major research interest is focused on dissecting pathomechanisms in neurodegenerative diseases such as Alzheimer’s and frontotemporal dementia (FTD), and exploiting molecular insight revealed toward development of therapies. He and his team use genetically modified model organisms and eemploynovel gene editing methods in order to improve these models. Key molecules of interest are tau, kinases such as Fyn and Pyk2, and amyloid-beta, and therapeutic strategies include small molecules, antibodies and peptides. The laboratory also strives to understand selective vulnerability in human neurodegenerative diseases, and to improve methods used to deliver therapeutic agents past the blood-brain barrier.
“With an ageing population placing an increasing burden on the health system, an important factor is cost, and other potential drug treatments using antibodies will be expensive,” Professor Götz observes. “In contrast, this method uses relatively inexpensive ultrasound and microbubble technology which is non-invasive and appears highly effective. The approach is able to temporarily open the blood-brain barrier, activating mechanisms that clear toxic protein clumps and restoring memory functions.With our approach the blood-brain barriers opening is only temporary for a few hours, so it quickly restores its protective role.”
Up to this point, the research has been conducted using mice with an Alzheimer’s model. The next step will be scaling up the research in higher animal models and eventually to conduct human clinical trials, which the scientists say are at least two years away.
“This treatment restored memory function to the same level of normal healthy mice,” Professor Götz adds. “We’re also working on seeing whether this method clears toxic protein aggregates in neurodegenerative diseases other than Alzheimers and whether this also restores executive functions, including decision-making and motor control.”
Sources:
University of Queensland
Science Translational Medicine
Clem Jones Centre for Ageing Dementia Research, Queensland Brain Institute
Australian Labor Party
Image Credits:
University of Queensland
Science Translational Medicine
Clem Jones Centre for Ageing Dementia Research, Queensland Brain Institute
Australian Labor Party






