Brain Imaging Can Help Distinguish Between Depression and Cognitive Disorders Like Alzheimer’s
Written by |
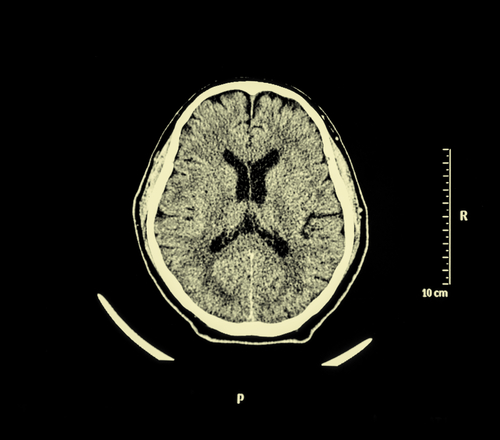
A brain imaging technique called single photon emission computed tomography, or SPECT, can help clinicians differentiate between depression and a cognitive disorder such as Alzheimer’s disease, according to new research.
The study, “ Classification of Depression, Cognitive Disorders, and Co-Morbid Depression and Cognitive Disorders with Perfusion SPECT Neuroimaging,” was published in the Journal of Alzheimer’s Disease.
Depression and cognitive disorders are two common co-morbid afflictions that present overlapping symptoms. But how can clinicians distinguish between both conditions?
“This is a critical clinical question that has practical implications for patient management and treatment,” Daniel G. Amen, MD, lead researcher and psychiatrist, said in a news release. “These disorders have very different prognoses and treatments and being able to improve diagnostic accuracy can improve outcomes for some patients.”
The researchers said cognitive impairment is present in about half of those who have late-onset depression, and depression is evident in 9 percent to 65 percent of people with dementia.
“Studies have indicated that the prevalence of depression in patients with mild cognitive impairment is 25%,” researchers wrote. “Consequently, it is often challenging to diagnostically disentangle depression and cognitive disorders from one another.”
Depression is usually diagnosed with tools such as the Beck Depression Inventory. But there was no significant difference in the burden of depression symptoms between people with both depression and cognitive disorders compared to those with either condition. This increases the difficulty of correctly diagnosing these disorders, based on the severity of depression symptoms alone.
SPECT imaging is a functional imaging technique performed to evaluate regional cerebral perfusion (blood flow). Because cerebral blood flow is closely linked to neuronal activity, the activity distribution is presumed to reflect neuronal activity levels in different areas of the brain.
“One of the greatest new insights of the past decade is the linkage of depression to the psychology of late life cognitive decline,” said George Perry, PhD, editor-in-chief of the Journal of Alzheimer’s Disease and dean and professor of biology at the University of Texas at San Antonio.
He said Cyrus Raji and his co-authors of the study “extend the approach to the biological substrate by an elegant imaging approach. These studies further place brain aging on a firm biological basis.”
The researchers examined 4,541 subjects, 847 of whom had dementia, 3,269 with depression, and 425 with both conditions. Diagnoses were made by board-certified or eligible psychiatrists, using all available data, including detailed clinical history, consistent with the current standard of care.
People with cognitive disorders had lower cerebral perfusion compared to those with depression. In those with both conditions, cerebral hypoperfusion was additive, with regions showing lower regional cerebral blood flow compared to either diagnosis alone.
The researchers also found that SPECT was able to differentiate depression from cognitive disorders with an accuracy of 86 percent. Furthermore, SPECT was able to distinguish depression or dementia in people with both conditions with an accuracy of 83 percent.
The results indicate that perfusion neuroimaging with SPECT can distinguish depression from dementia, and may help clinicians more accurately diagnose these two disorders.





