Design Of Micro And Nanoparticles To Improve Treatments For Alzheimer’s and Parkinson’s Diseases
At the Faculty of Pharmacy of the University of the Basque Country (Basque – Euskal Herriko Unibertsitatea; Spanish – Universidad del Pas Vasco – UPV/EHU) in Leioa, northern Spain, encapsulation techniques are being developed to deliver correctly and effectively certain drugs used to treat neurological diseases. Enara Herran, a researcher at the University of the Basque Country’s Departments of Pharmacy and Pharmaceutical Technology, is working to improve the way Alzheimer’s and Parkinson’s treatments are administered, observing understatedly that, “both diseases are becoming more and more common in our society.”
Both Alzheimer’s and Parkinson’s affect key components of the nervous system called neurones (also known as a neuron or nerve cell) — electrically excitable cells that process and transmit information through electrical and chemical signals. In these diseases, neurone structure and function are lost, in turn leading to deterioration in the patient’s motor, cognitive, sensory and emotional functions.
As Dr. Herran points out in a UPV/EHU release, in many cases drugs used to treat both Alzheimer’s and Parkinson’s only mitigate the symptoms; they do not act on the origin of the disease. “The treatment is usually on the basis of tablets taken by mouth.”
However, drugs of this type are not the only ones used to tackle both Alzheimer’s and Parkinson’s. Some drugs prevent neuron loss and help new ones to form; growth factors, for example. “In any case, they are not used so much because there is no effective, safe way of delivering them,” explains Dr. Herran, noting that the drugs have to pass through the blood-brain barrier to reach the neurons, and that is no straightforward task. This is in fact the problem Dr. Herran is seeking to overcome by means of her research.
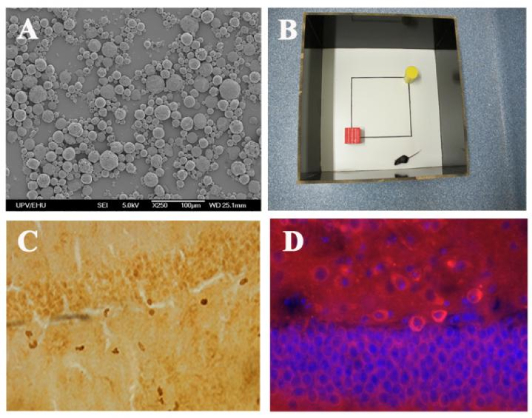
“Growth factors are encapsulated so that they can be administered more effectively and more safely. In other words, they are inserted into micro and nanocapsules and implanted in the brain by means of craniotomy. That way, the drugs would be released right where they have to act, and what is more, in an ongoing way and in the correct dose,” explains Dr. Herran. The micro and nanoparticles release these growth factors within a period ranging from 2-3 months and one year until the polymer has degraded. That way the patient does not have to take the medication every day. In any case, this is not the only advantage. In experiments carried out on rats and mice the encapsulated drugs have been found to be much more effective than those taken by mouth. As Herran pointed out, “these two diseases are already a problem for public health, and the scientific community is making a great effort in the quest for and in advances in new treatments.”
As Dr. Herran explained, in experiments conducted on animals they have tested two factors the vascular endothelial growth factor (VEGF) and the glial cell-line derived neurotrophic factor (GDNF) encapsulated in a biocompatible, biodegradable polymer poly (lactic co-glycolic acid) (PLGA). “We obtained micro and nanoparticles using various encapsulation techniques. Initially, we did the tests for Parkinson’s; first in cell cultures and then on mice. We got good results in both trials,” she observes. Dr. Herran stresses that the mice treated with particles improved considerably: “A great improvement was noted in comparison with the control group in terms of behavior as well as the healing of the damaged zones.”
After that, they carried out the test for Alzheimer’s in mice. Herran said that in this case they also achieved good results: “Three months after having carried out the procedure, the mice treated had good memories; similar to those of healthy mice. Through a histological analysis we found that the beta-amyloid plaques that develop in Alzheimer’s had diminished considerably and so had the inflammation, and that angiogenesis had intensified.”
The results and conclusions of these experiments have been publicized in specialized publications including the renowned Journal of Controlled Release. And this is in fact the subject of her PhD thesis. Although the research has not been completed, Herran said she is now doing research into the way of obtaining “better formulations,” so as not to have to implant the micro and nanoparticles in the brain. The final goal is clear: to develop the most effective, safest and most suitable way of treating Parkinson’s and Alzheimer’s.
The University of the Basque Country (Basque – Euskal Herriko Unibertsitatea; Spanish – Universidad del Pas Vasco) is the only public university in the Basque Country, in Northern Spain. It has campuses over the three provinces of the autonomous community: Biscay Campus (in Leioa, Bilbao, Portugalete and Barakaldo), Gipuzkoa Campus (in San Sebastin and Eibar), and lava Campus in Vitoria-Gasteiz. It is the main research institution in the Basque Country, carrying out 90% of the basic research made in that territory and taking advantage of the good industrial environment that the region constitutes.
Enara Herran-Martnez (Vitoria-Gasteiz, 1985), a Doctor in Pharmacy, wrote up her PhD thesis on “Micro y nanopartculas de factores angiognicos y neurotrficos como herramienta teraputica para el tratamiento de enfermedades neurodegenerativas” (Micro and nanoparticles of angiogenic and neurotrophic factors as a therapeutic tool for treating neurodegenerative diseases), under the supervision of Prof Rosa Mara Hernndez and Dr Manoli Igartua, of the UPV/EHU’s Department of Pharmacy and Pharmaceutical Technology.
She produced her thesis mainly in the UPV/EHU’s Department of Pharmacy and Pharmaceutical Technology, although part of it was done in the Neurosciences Laboratory at the research centre of the Hospital 12 de Octubre in Madrid.
In connection with her thesis Dr. Herran-Martnez has had various papers published in scientific journals:
E. Herran, J.A. Ruis-Ortega, A. Aristieta, M. Igartua, C. Requejo, J.V. Lafuente, L. Ugedo, J.L. Pedraz, R.M. Hernandez. “In vivo administration of VEGF- and GDNF-releasing biodegradable polymeric microspheres in a severe lesion model of Parkinson’s disease”. European Journal of Pharmaceutics and Biopharmaceutics 85 – 3: 1183 – 1190 (2013).
E. Herran, R. Perez-Gonzalez, M. Igartua, J.L. Pedraz, E. Carro, R.M. Hernandez. “VEGF-releasing biodegradable nanospheres administered by craniotomy: A novel therapeutic approach in the APPPs1 mouse model of AD”. Journal of Controlled Release 170: 111 – 119 (2013).
E. Herran, C. Requejo, J.A. Ruiz-Ortega, A. Aristieta, M. Igartua, H. Bengoetexea, L.Ugedo, J.V. Lafuente, R.M. Hernandez. “Increased antiparkinson efficacy of the combined administration of VEGF and GDNF-releasing nanospheres in a partial lesion model of Parkinson’s disease”. International Journal of Nanomedicine 9: 2677 – 2687 (2014).
E. Herran Martinez, M. Igartua Olaechea, J.L. Pedraz Muoz, R.M. Hernndez Martin. “Novel Drug Delivery Systems for Releasing Growth Factors to the CNS: Focus on Alzheimer’s and Parkinson’s Diseases”. Mini-Reviews in Medicinal Chemistry 14 – 7: 557 – 566 (2014).
UCLA Team Find Drug Used For Another Disease Slows Progression Of Parkinson’s
In related research, new study from UCLA has found that a drug being evaluated to treat an entirely different disorder helped slow the progression of Parkinson’s disease in mice.
The study, published in the October edition of the journal Neurotherapeutics, found that the drug, AT2101, which has also been studied for Gaucher disease, improved motor function, stopped inflammation in the brain and reduced levels of alpha-synuclein, a protein critically involved in Parkinson’s.
Although the exact cause of Parkinson’s is unknown, evidence points to an accumulation of alpha-synuclein, which has been found to be common to all people with the disorder. The protein is thought to destroy the neurons in the brain that make dopamine, a neurotransmitter that helps regulate a number of functions, including movement and coordination. Dopamine deficiency is associated with Parkinson’s disease.
Gaucher disease is a rare genetic disorder in which the body cannot produce enough of an enzyme called beta-glucocerebrosidase, or GCase. Researchers seeking genetic factors that increase peoples risk for developing Parkinson’s have determined that there may be a close relationship between Gaucher and Parkinson’s due to a GCase gene. Mutation of this gene, which leads to decreased GCase activity in the brain, has been found to be a genetic risk factor for Parkinson’s, although the majority of patients with Parkinson’s do not carry mutations in the Gaucher gene.
 This is the first time a compound targeting Gaucher disease has been tested in a mouse model of Parkinson’s disease and was shown to be effective, said the study’s senior author, Marie-Francoise Chesselet, the Charles H. Markham Professor of Neurology at UCLA and director of the UCLA Center for the Study of Parkinson’s Disease part of the UCLA Department of Neurology, which encompasses more than 26 disease-related research programs. The promising findings in this study suggest that further investigation of this compound in Parkinson’s disease is warranted.
This is the first time a compound targeting Gaucher disease has been tested in a mouse model of Parkinson’s disease and was shown to be effective, said the study’s senior author, Marie-Francoise Chesselet, the Charles H. Markham Professor of Neurology at UCLA and director of the UCLA Center for the Study of Parkinson’s Disease part of the UCLA Department of Neurology, which encompasses more than 26 disease-related research programs. The promising findings in this study suggest that further investigation of this compound in Parkinson’s disease is warranted.
In the study, the researchers used mice that were genetically engineered to make too much alpha-synuclein which, over time, led the animals to develop deficits similar to those observed in humans with Parkinson’s. The researchers found that the mices’ symptoms improved after they received AT2101 for four months.
The researchers also observed that AT2101 was effective in treating Parkinson’s in mice even though they did not carry a mutant version of the Gaucher gene, suggesting that the compound may have a clinical effect in the broader Parkinson’s population.
AT2101 is a first-generation pharmacological chaperone a drug that can bind malfunctioning, mutated enzymes and lead them through the cell to their normal location, which allows the enzymes to carry on with their normal work. This was the first time that a pharmacological chaperone showed promise in a model of Parkinson’s, according to Chesselet.
Parkinson’s disease affects as many as 1 million Americans, and 60,000 new cases are diagnosed each year. The disorder continues to puzzle scientists. There is no cure and researchers have been unable to pin down its cause and no drug has been proven to stop the progression of the disease, which causes tremors, stiffness and other debilitating symptoms. Current Parkinson’s treatments only address its symptoms.
The research was supported by Amicus Therapeutics, the UCLA Morris K. Udall Parkinson’s Disease Research Center of Excellence (NIH grant NS-P50 NS38367), and gifts to the UCLA Center for the Study of Parkinson’s Disease. A complete list of authors and additional disclosures are available in the manuscript.
Sources:
The University of the Basque Country
UCLA
Image Credits:
The University of the Basque Country
UCLA






