Differences Seen in How Amyloid Builds on Blood Vessels and on Neurons
Written by |
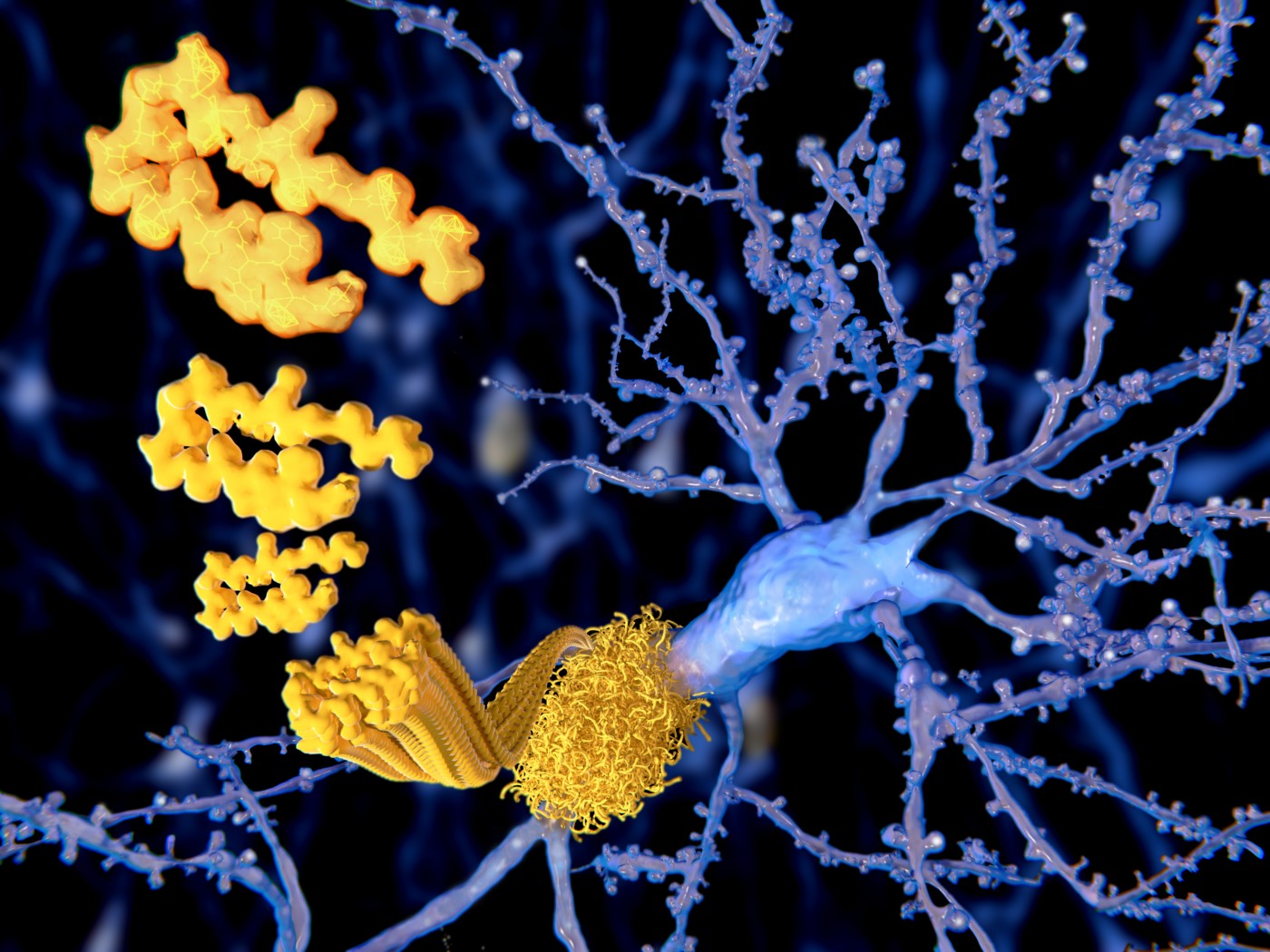
Researchers have discovered that amyloid-beta — the protein that builds in the brain of Alzheimer’s disease patients — has different structures when it accumulates around blood vessels and neurons.
Although the researchers could not conclude how these differences impact the disease, they believe that amyloid buildup around blood vessels differs in its impact from the protein aggregates around neurons.
The study, “Cerebral vascular amyloid seeds drive amyloid β-protein fibril assembly with a distinct anti-parallel structure,” was published in the journal Nature Communications.
The existence of amyloid-beta aggregates surrounding blood vessels has been known for a while. Many Alzheimer’s disease patients have protein buildup both in brain tissue and around vessels.
Some forms of familial Alzheimer’s are also caused by mutations that specifically lead to the protein accumulating around blood vessels, a condition called cerebral amyloid angiopathy.
Earlier studies have shown that blood vessel-specific amyloid contributes to cognitive decline by triggering damaging events such as inflammation, poor blood flow, and low tissue-oxygen levels. Scientists have also reported that natural antibodies react differently to amyloid collecting around blood vessels and around neurons, suggesting that the two protein types differ.
Researchers at Stony Brook University in New York used genetically engineered mice to show that the two types of amyloid have different structures.
Neuronal amyloid was organized in what researchers call a parallel, in-register orientation, with all amyloid proteins lined up the same way.
Amyloid that surrounded blood vessels, however, showed strands organized in alternating opposite directions — a structure researchers refer to as antiparallel.
Importantly, the research team also demonstrated that mutant amyloid from mice that model cerebral amyloid angiopathy speed up the aggregation of normal amyloid. The finding further supports previous observations that proteins in diseases such as Alzheimer’s can behave as prions — where a faulty protein can trigger the misfolding and aggregation of normal proteins.
“This discovery may help guide us to the development of a new diagnostic tool or therapeutic intervention for dementia patients who display this vessel pathology,” William Van Nostrand, PhD, a professor in the Department of Neurosurgery and the study’s senior investigator, said in a news release.





