Discovery of Stem Cells in Brain Membranes May Offer New Paths in Alzheimer’s Research
Written by |
Scientists have found that the membranes covering the brain — once believed to have little influence on the workings of the organ inside — are housing stem cells.
The discovery is likely to advance research into stem cell therapies for brain regeneration, an attractive but so far unreachable treatment option for Alzheimer’s disease.
While the study, “Neurogenic Radial Glia-like Cells in Meninges Migrate and Differentiate into Functionally Integrated Neurons in the Neonatal Cortex,” which recently appeared in the journal Cell Stem Cell, is likely to boost stem cell research, the authors admit that plenty of work remains to be done before the power of the newfound cells can be harnessed.
A few decades ago, the realization that neuron-producing stem cells exist in the brain revolutionized the way scientists viewed brain damage. Although researchers once believed the brain developed only until adult age, they started realizing it had some regenerative power. With that insight came attempts to use stem cells to regenerate brain tissue lost to diseases like Alzheimer’s.
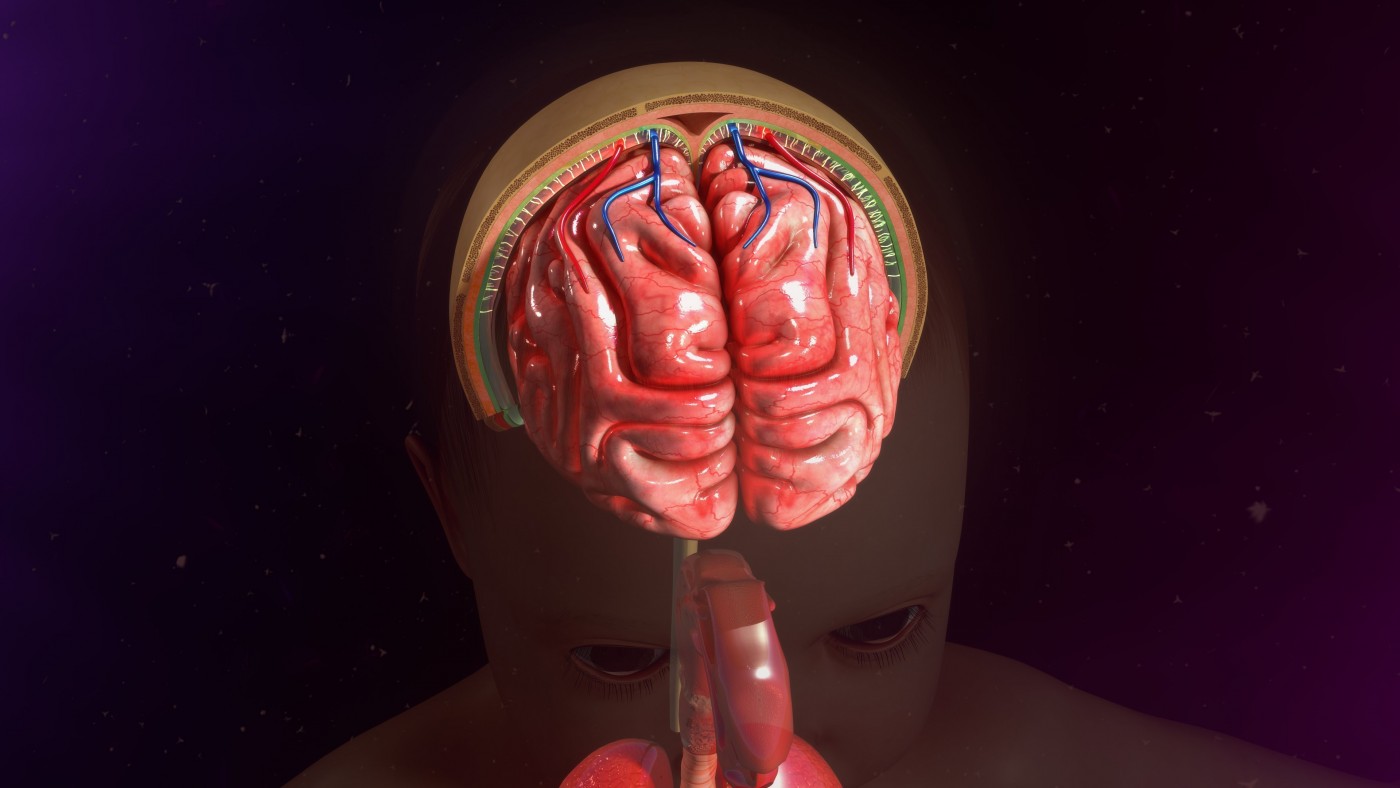
Until now, researchers believed that stem cells existed only in the brain tissue itself. Researchers at the Flanders Institute for Biotechnology (VIB), led by Dr. Peter Carmeliet, changed that longstanding belief when they discovered that the meninges — membranes separating the brain from the skull — of newborn mice contain stem cells.
The team observed how the cells traveled to various parts of the brain and became integrated into neural circuits as mature neurons. They were aided in their experiments by a new technology that made it possible to analyze the entire set of RNA (ribonucleic acid) molecules in a single cell at a given time.
Since RNA acts as a messenger between genes and proteins, the analysis gives scientist a snapshot of the activity of all genes in that cell — information that allows researchers to distinguish a stem cell from an immature or mature neuron.
“An intriguing question is whether these neuronal stem cells in the meninges could lead to better therapies for brain damage or neurodegeneration,” Carmeliet, professor at VIB-KU Leuven and the study’s senior author, said in a news release.
But as with other types of stem cells, researchers first have to study and learn to control the factors that prompt a stem cell to transform into various types of neurons before such an idea can become reality.
“Can we therapeutically ‘hijack’ their regeneration potential to restore dying neurons in, for example, Alzheimer’s disease, Parkinson’s disease, [ALS] and other neurodegenerative disorders? These findings open up very exciting research opportunities for the future,” Carmeliet said.





