Fungal Infection as a Risk Factor in Alzheimer’s Disease
Written by |
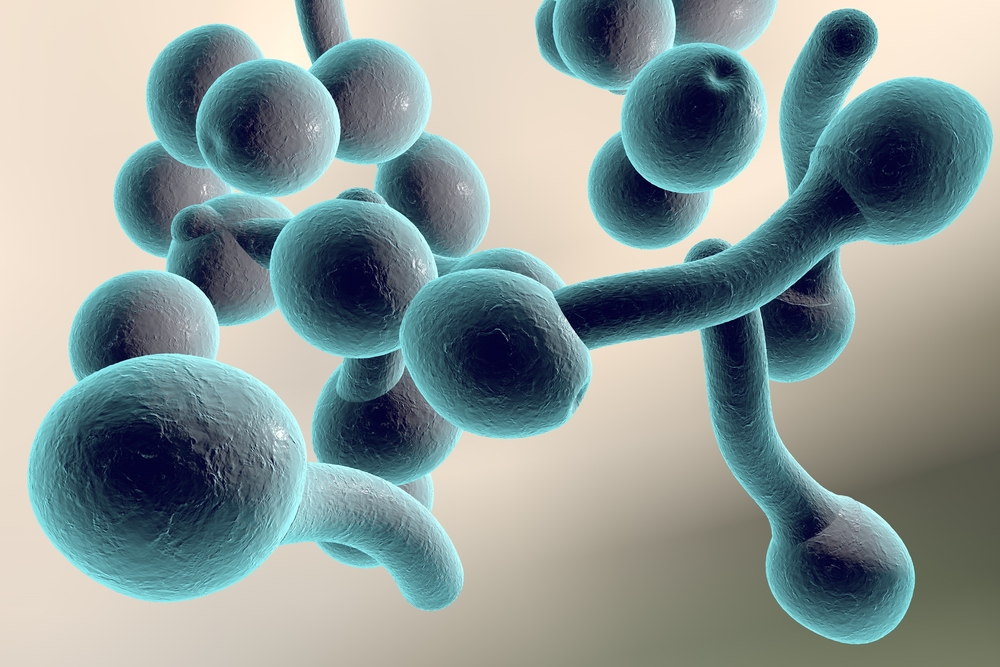
A new study reports the finding of fungal cells and hyphae in tissue from different regions of the central nervous system (CNS) in Alzheimer’s disease (AD) patients. The research article, entitled “Different Brain Regions are Infected with Fungi in Alzheimer’s Disease”, was published in Scientific Reports.
AD patients present aggregates of misfolded proteins in different part of the CNS, a common feature shared with other neurodegenerative diseases such as multiple sclerosis (MS), Parkinson’s disease (PD), and amyotrophic lateral sclerosis (ALS). Specifically, AD is characterized by the presence of extracellular deposits of amyeloid protein and intracellular accumulation of hyperphosphorilated tau protein. The precise cause of AD is still poorly understood although researchers have formulated different cause conjectures, such as the “amyeloid hypothesis” and the autoimmune cause, with no definitive agreement. One hypotheses relates AD pathogenesis to an infectious cause or infectious disease as a risk factor. This conjecture stems from several studies reporting genetic material of viruses and bacteria found in AD patients’ brains, namely herpes simplex type 1 (HSV-1) and Chlamydophila pneumoniae.
This study included samples of frozen brain tissue from 11 patients plus four patients previously analyzed. Through several assays and molecular techniques, such as immunohistochemistry and immunofluorescence analysis of tissue sections and DNA PCR amplification and sequencing, researchers identified fungal cells both intracellularly and extracellularly, while there was no detection in control patients. Furthermore, fungal polysaccharides, proteins and DNA were detected in the blood serum of the AD patients. Fungal proteins and DNA were also detected in the patients’ brain tissue. The results from this research are corroborated by other institutions’ research, where, for example, chitin, a polymer found on fungi cell walls, was detected in AD brains and the chitinase enzyme was found in patients’ blood serum and cerebrospinal fluid.
If fungal infection is indeed related to AD pathogenesis, these results can have two different interpretations. Either the untreated infection is indeed a cause for the slow onset of neurodegeneration, for example through inflammation and immune system activation, or patients experiencing fungal infections are more vulnerable to the disease. Further research is therefore needed to uncover the cause of AD, including testing the possible role of fungal infection, and, consequently, to develop therapies that treat its cause, instead of only mitigating its symptoms.





