New Direction in Alzheimer’s Research May Help Identify Origin of Disease
The study of axonal transport, the system responsible for transporting vital molecules and signals from one nerve cell to another, may lead scientists to the origin of Alzheimer’s disease, according to researchers at the University at Buffalo, New York.
Malfunctions in this transport system create “traffic jams,” and these may be the start of the formation of toxic plaques — the buildup of beta-amyloid proteins that are one of the most characteristic traits of Alzheimer’s.
Over the past 20 years, Alzheimer’s research has been focused on the formation of beta-amyloid plaques in patients’ brains. Many researchers believe that blocking the formation or removing these plaques may help in slowing disease progression.
But several clinical trials based on these approaches failed, and some researchers are now questioning this premise. They are suggesting other hypotheses to explain the origin of Alzheimer’s that may potentially help in the development of new treatments.
Such is the case of Shermali Gunawardena, PhD, an associate professor of biological sciences at the University of Buffalo. Her team is focused on the role of presenilin, a protein involved in the generation of beta-amyloid plaques, in axonal transport.
“We are looking at processes that occur before cell death, before you start to see plaques in the brain,” Gunawardena said in a press release. “A lot of the treatments being developed for Alzheimer’s are targeting beta-amyloid, but maybe we should be targeting processes that happen earlier on, before plaques are formed.”
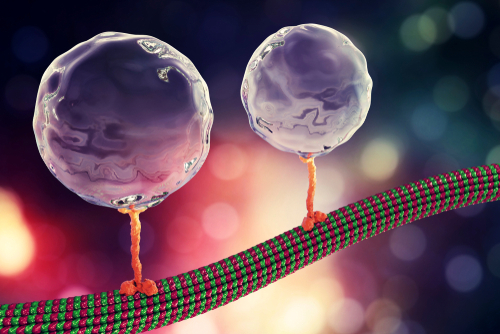
Years of research by Gunawardena’s lab demonstrated that presenilin acts as a traffic controller by regulating the flow of traffic in the neurons of the fruit fly. Specifically, presenilin affects how quickly molecular motors — protein structures responsible for movement — travel along neuronal pathways called microtubules.
Recently, researchers showed that presenilin works alongside an enzyme called GSK-3β to control motor movement and how it binds to vesicles — structures that carry proteins and other molecules needed for neuron survival and function.
In their latest study, “The presenilin loop region is essential for glycogen synthase kinase 3 β (GSK-3β) mediated functions on motor proteins during axonal transport,” published in the journal Human Molecular Genetics, the research team explains how presenilin interacts with GSK-3β and demonstrates the importance of a molecular structure within presenilin, a loop region, on proper traffic control.
“Our observations together with previous work that showed that the loop region of presenilin interacts with GSK-3β propose a scaffolding mechanism for presenilin in which the loop region sequesters GSK-3β away from motors for the proper regulation of motor function,” researchers wrote.
The team’s findings showed that presenilin has two antagonist roles in Alzheimer’s. On the one hand, the protein helps in the production of beta-amyloid plaques in patients’ brains; on the other, presenilin regulates the flow of traffic in neurons, preventing failures that can cause cell death and disease.
The last may be a possible reason to justify why genetic mutations that result in a loss of fuction of presenilin may lead to Alzheimer’s.
“We are curious about the normal function of presenilin,” Gunawardena said. “What does this protein normally do? In the past, we have thought of it as being implicated in the production of beta-amyloid, but in fact, presenilin appears to also have a very different function independent of this.
“As we learn more about presenilin, it’s possible that our research will result in new, more targeted opportunities for treating or preventing Alzheimer’s disease,” she added.






