ProMIS’ PMN310 Shows Improved Safety Profile, Specificity Compared to Similar Alzheimer’s Candidates
Written by |
ProMIS Neurosciences’ lead therapeutic candidate for Alzheimer’s disease, PMN310, showed an improved safety profile when directly compared to other amyloid-beta directed antibodies, according to preclinical study results.
Unlike BAN2401 (Biogen, Eisai) and aducanumab (Biogen), two amyloid-beta directed antibodies both in clinical development, PMN310 did not bind to nontoxic forms of amyloid beta in the Alzheimer’s brain, displaying an increased specificity for soluble toxic amyloid beta oligomers.
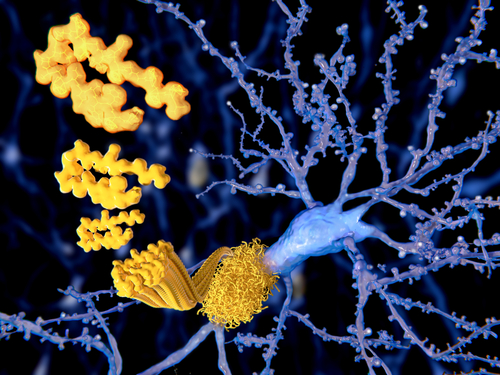
Alzheimer’s disease is thought to develop as a consequence of deposits of toxic clumps of the mutant form of amyloid beta protein within the nerve cells of the brain.
The brain has three forms of amyloid beta. The toxic form that kills nerve cells and promotes neurodegenerative disease is the oligomer form. Oligomers are a smaller, more toxic version of plaques.
Binding of therapeutic antibodies to amyloid beta deposits in brain tissue, particularly in blood vessels, is though to be the underlying cause of the development of ARIA (amyloid-related imaging abnormalities; brain swelling and micro-hemorrhages) in treated Alzheimer’s patients.
PMN310 is a humanized antibody that attacks only toxic forms of the amyloid beta protein linked to Alzheimer’s, not its normal forms.
“PMN310 was designed to selectively target soluble toxic [amyloid beta] oligomers, now widely believed to be a root cause of [Alzheimer’s disease],” ProMIS president and CEO Elliot Goldstein, MD, said in a press release.
BAN2401 and aducanumab appear to target both amyloid-beta plaque and soluble amyloid-beta oligomers. Results from recent clinical trials have shown that both therapies are associated with dose-limiting brain swelling in a significant number of Alzheimer’s patients.
The capacity of PMN310 to selectively target toxic amyloid-beta oligomers and not amyloid-beta plaque, shown in different preclinical studies, may allow for the safe administration of higher effective doses than those observed with BAN2401 or aducanumab.
ProMIS presented a scientific poster during the Alzheimer’s Association International Conference (AAIC), held July 22-26 in Chigaco, titled, “Humanized PMN310 shows enhanced therapeutic potential by binding toxic low molecular weight Aβ oligomers while avoiding ARIA-related binding to Aβ deposits in AD patient brains,” which adds to the company’s data.
“Confirmation of such an improved safety profile in clinical trials would allow for administration of higher doses to [Alzheimer’s] patients, thereby potentially leading to greater therapeutic potency of PMN310,” Goldstein said.
Researchers compared the binding profile of PMN310 in human Alzheimer’s brain tissues directly to that of BAN2401 and aducanumab using a technique called immunohistochemistry (IHC).
IHC is the process of imaging proteins in biological tissue (in this case, amyloid-beta plaques in Alzheimer’s brain tissue) through the use of antibodies that can bind to those same proteins.
Results from this study indicated that while BAN2401 and aducanumab bind to amyloid-beta plaques throughout the brain (especially in blood vessels), PMN310 did not bind to amyloid-beta plaques in any region of Alzheimer’s brain tissues.
These findings add to previous study results which show that PMN310 has a greater selectivity for amyloid-beta oligomers compared to aducanumab.
“Although both BAN2401 and aducanumab have shown encouraging Phase 2 clinical results, the greater selectivity and avoidance of plaque binding with PMN310 may confer significant advantages in the clinic supporting PMN310 as potential ‘best in class’ therapy,” Goldstein added.
ProMIS has announced PMN310 is expected to enter clinical Phase 1 trials in 2019.





