Scientists Develop An Early Warning Gene Signature For Alzheimer’s
Written by |
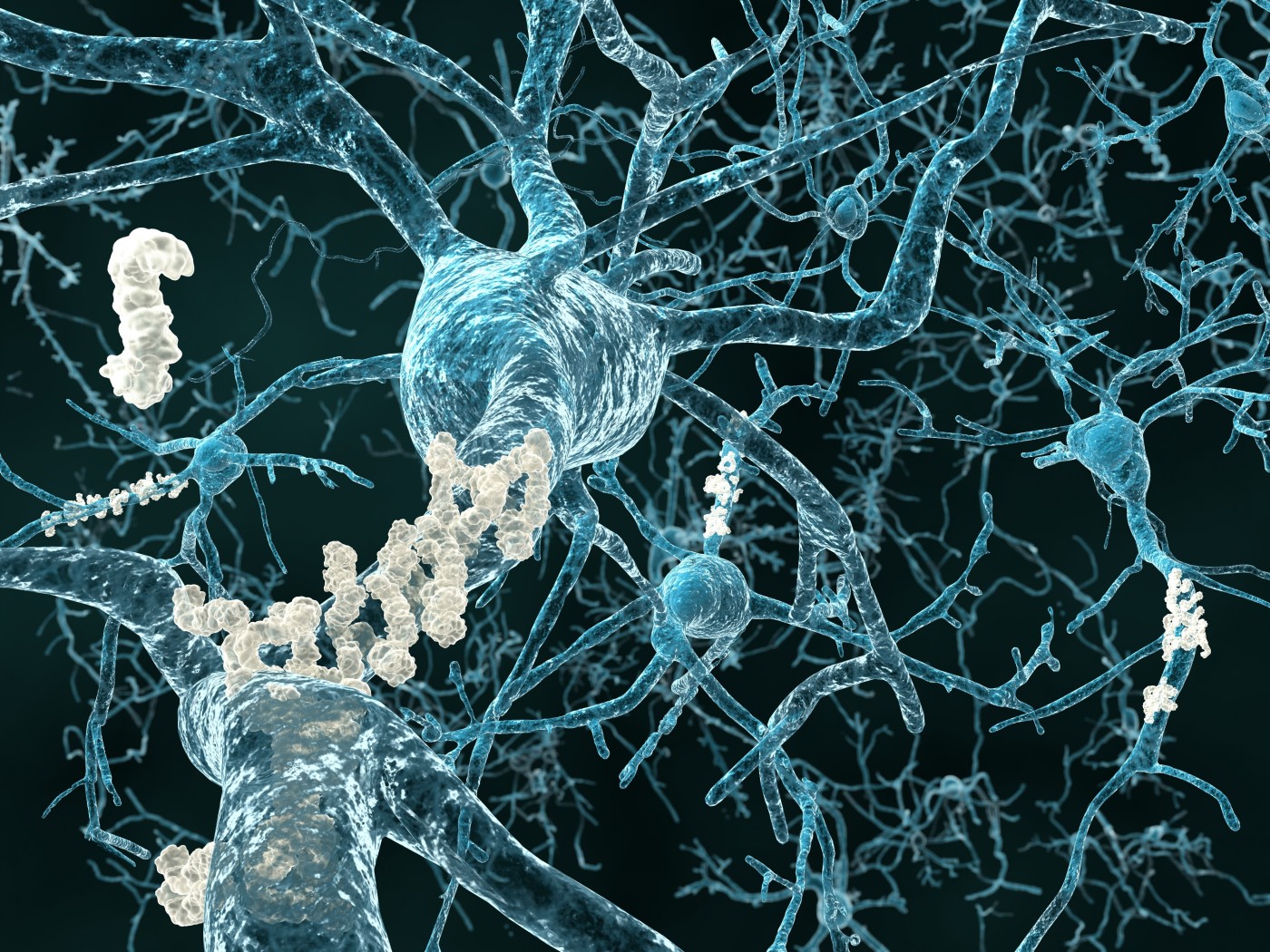
A gene signature that could be used to predict the onset of diseases, such as Alzheimer’s, years in advance has been developed in a study published in the open access journal Genome Biology.
The objective of the study, entitled “A novel multi-tissue RNA diagnostic of healthy ageing relates to cognitive health status“ (Genome Biology 2015, 16:185 doi:10.1186/s13059-015-0750-x), was to define a set of genes associated with healthy ageing in 65 year olds — molecular profiling that could be useful for distinguishing people at earlier risk of age-related diseases and a substantial improvement over reliance on chronological age and complementary traditional indicators of disease, such as blood pressure.
The researchers note that improved diagnostics of the human aging process may help predict future healthcare needs or guide preventative measures for tackling diseases associated with older age.
The scientists explain that they used transcriptomics; study of the transcriptome — the complete set of RNA transcripts (eg: mRNA, rRNA, tRNA and others) — that are produced by the genome under specific circumstances or in a specific cell using high-throughput methods, such as microarray analysis. They used this method to build the first reproducible multi-tissue RNA expression signature by gene-chip profiling tissue from sedentary normal subjects who had reached 65 years of age in good health, and used the information to develop a signature of 150 RNA genes that indicated healthy ageing.
With this RNA signature, which was found to be a reliable predictor for risk of age-related disease when studying RNA from tissues including human muscle, brain and skin, they developed a healthy age gene score which they used to test and compare the RNA profiles of different individuals, for example demonstrating that greater scores were associated with better health in both men and women.
The researchers studied RNA from healthy 70 year old subjects and analyzed follow-up health data over two decades. Despite all subjects being born within a year of each other, their RNA at around 70 years of age demonstrated a broad distribution in healthy age gene score, varying over a four-fold range. This variation was shown to be relevant to long term health, with greater gene scores also associated with better cognitive health and renal function across a 12 year span — both factors being important determinants of mortality. In particular, it was demonstrated that patients diagnosed with Alzheimer’s Disease had an altered healthy ageing RNA signature in their blood, and therefore a lower healthy age gene score, suggesting significant association with the disease.
Using the Uppsala Longitudinal Study of Adult Men birth-cohort, the investigators demonstrate that the RNA classifier is insensitive to confounding lifestyle biomarkers, while greater gene score at age 70 years is independently associated with better renal function at age 82 years and longevity. The gene score is up-regulated in healthy human hippocampus with age, and when applied to blood RNA profiles from two large independent age-matched dementia casecontrol data sets the scientists found that healthy controls have significantly greater gene scores than those with cognitive impairment. They observe that either alone, or when combined with their previously described prototype Alzheimer’s disease (AD) RNA disease signature, the healthy ageing RNA classifier is diagnostic for AD.
RELATED :Alzheimer’s Disease Brain Deficits Reversed in Mouse Model By Yale School of Medicine
The researchers conclude that their identification of a novel and statistically robust multi-tissue RNA signature of human healthy ageing can serve as a diagnostic of future health, using only a peripheral blood sample, and project that this RNA signature has great potential to assist research aimed at finding treatments for and/or management of AD and other ageing-related conditions, especially with neurological decline projected to contribute substantially to the economic burden of healthcare in the coming decades, and AD being a multi-factorial disease with some 22 genetic loci potentially associated with disease risk or progression of symptoms.
The coauthors observe that in general, molecular mechanisms that define healthy ageing in both human and animal models remain elusive, with such mechanisms observed to extend the lifespan of laboratory animals also appearing to extend health-span or disease-free ageing in these models. However, they say it remains unclear as to whether any of these mechanisms are central to human ageing or define healthy ageing in humans. They observe that their approach was novel in that they first sought to define a set of genes associated with healthy ageing in normal 65-year-old subjects rather than gene expression associated with disease or extreme longevity — an important distinction because ageing is thought to be a continuous physiological process that could be expected to have a gene expression signature distinct from lifestyle related (e.g., type II diabetes) or mutation driven (e.g., cancer) pathologies, thus explaining its independent prognostic rather than specific diagnostic capacity.
The team say it is of potential importance that regulation of the healthy ageing signature in human brain is most evident in those regions associated with neurodegeneration, while in contrast, it is thought that the cerebellar cortex is not subject to substantial age-related anatomical changes — a deduction consistent with their new model of human healthy ageing. They suggest that the RNA diagnostic could be used to facilitate evaluation of anti-ageing-related treatments in middle-aged humans, to screen for long-term safety during drug development, or to augment clinical decision-making that currently inputs chronological age, rather than biological age, into treatment algorithms, and that future efforts should focus on discovering strategies to modulate the healthy ageing gene signature in order to establish whether it is causally determining health or just acting as a robust biomarker of a more complex set of molecular interactions.
The investigators point to exceptional longevity being driven by a measurable genetic contribution, while being active and healthy at age 65 years is a more common occurrence, likely to reflect complex molecular factors, and less obviously linked to only variations in DNA sequence. Consequently they say the healthy ageing gene expression signature has the key advantage of being built using a paradigm and samples entirely distinct from AD case control samples,and that the healthy ageing gene score allowed them to demonstrate that patients diagnosed with AD have an altered healthy ageing RNA expression signature in blood that demonstrates significant association with disease. Furthermore, the muscle or blood gene score was unrelated to lifestyle diseases such as type II diabetes and thus may be more clinically specific than earlier AD biomarkers, most of which did not replicate in independent clinical studies.
 Study co-lead author James Timmons, a Professor of Precision Medicine at King’s College London, UK, notes in a release: “We use birth year, or chronological age, to judge everything from insurance premiums to whether you get a medical procedure or not. Most people accept that all 60 year olds are not the same, but there has been no reliable test for underlying ‘biological age’. Our discovery provides the first robust molecular signature of biological age in humans and should be able to transform the way that ‘age’ is used to make medical decisions. This includes identifying those more likely to be at risk of Alzheimer’s, as catching those at ‘early’ risk is key to evaluating potential treatments.”
Study co-lead author James Timmons, a Professor of Precision Medicine at King’s College London, UK, notes in a release: “We use birth year, or chronological age, to judge everything from insurance premiums to whether you get a medical procedure or not. Most people accept that all 60 year olds are not the same, but there has been no reliable test for underlying ‘biological age’. Our discovery provides the first robust molecular signature of biological age in humans and should be able to transform the way that ‘age’ is used to make medical decisions. This includes identifying those more likely to be at risk of Alzheimer’s, as catching those at ‘early’ risk is key to evaluating potential treatments.”
Dr. Timmons continues: “This is the first blood test of its kind that has shown that the same set of molecules are regulated in both the blood and the brain regions associated with dementia, and it can help contribute to a dementia diagnosis. This also provides strong evidence that dementia in humans could be called a type of accelerated ageing or failure to activate the healthy ageing program.”
Like many genomic diagnostics, the researchers say the full clinical utility of theirs will only emerge when combined with additional data and clinical insight, and that while they could also demonstrate that patients with mild cognitive impairment (MCI) had a significantly lower healthy ageing gene score, it remains to be demonstrated that these data can be converted into a diagnostic for future cognitive health. However the coauthors suggest that given the importance of early intervention in Alzheimer’s and a need to identify those at greatest risk, their healthy ageing gene score could be integrated to help decide which middle-aged subjects could be offered entry into preventative clinical trials many years before clinical expression of Alzheimer’s.
Sources:
Genome Biology serves the biological research community as an international forum for the dissemination, discussion and critical review of information about all areas of biology informed by genomic research. Genome Biology key objectives are to provide a guide to the rapidly developing resources and technology in genomics and its impact on biological research, to publish large datasets and extensive results that are not readily accommodated in traditional journals, and to help establish new standards and nomenclature for post-genomic biology.
BioMed Central is a Science, Technology and Medicine (STM) publisher that is pioneering the open access publishing model. All peer-reviewed research articles published by BioMed Central are made immediately and freely accessible online, and licensed to allow redistribution and reuse. BioMed Central is part of Springer Science+Business Media, a leading global publisher in the STM sector. For more information, visit: https://www.biomedcentral.com





