USC Joins Consortium to Look for Blood-vessel-related Biomarkers of Alzheimer’s
Written by |
The University of Southern California’s Keck School of Medicine has joined a nationwide consortium of researchers looking for biological factors that could help predict blood-vessel-related health conditions, including dementia and Alzheimer’s.
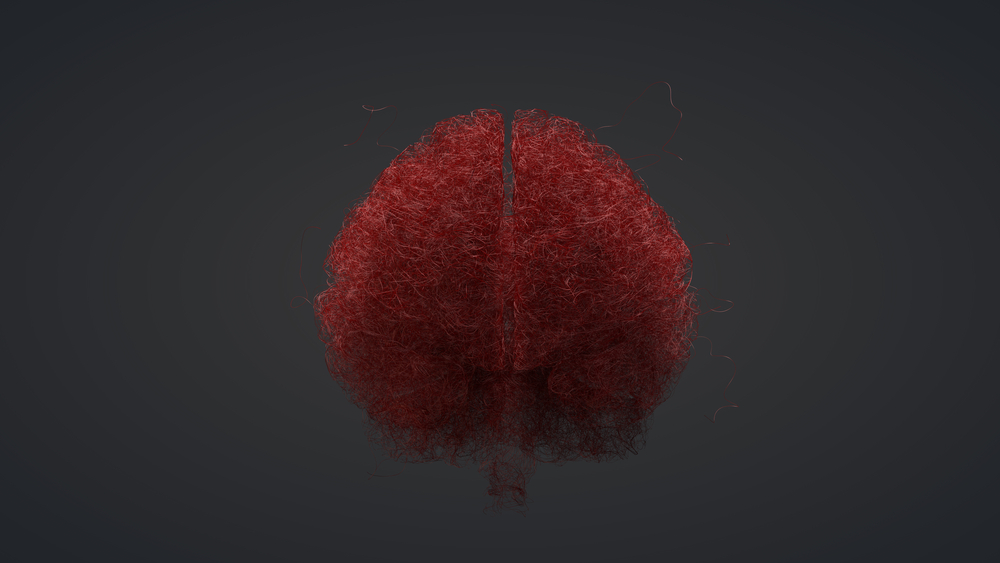
Six institutions besides USC are part of the initiative that the National Institutes of Health started two years ago. Scientists are studying the role that small blood vessel diseases in the brain play in cognitive impairment and dementia with an eye toward developing biomarkers for them.
The ultimate goal of the NIH-sponsored research is to help doctors do a better job of diagnosing and predicting the outcomes of these disorders. NIH has dubbed the initiative MarkVCID, for Biomarkers for Vascular Contributions to Cognitive Impairment and Dementia.
Two NIH branches — the National Institute of Neurological Disorders and Stroke and the National Institute on Aging — are putting up the $6 million in funding for the five-year program.
USC and the other six institutions are trying to improve on current blood-vessel-related biomarkers of cognitive impairment and dementia, and come up with new ones. A center at Massachusetts General Hospital in Boston is coordinating the work.
“We all know that dementia is a tsunami waiting to happen,” Steven Greenberg, principal investigator at the Boston center, said in a USC news story. “It’s going to be a true public health emergency.”
Scientists need to understand “what role damage to small blood vessels plays in the bigger picture,” he said. “We’re committed to finding biomarkers that don’t just look promising, but are really ready for prime time, ready to be immediately plugged into clinical trials.”
Researchers are obtaining information from a number of sources. They include brain scans, genetic profiles, patients’ symptoms, neuropsychological assessments and fluid samples, such as cerebrospinal fluid and blood.
USC will be examining the permeability of the blood-brain barrier, which the body uses to try to keep harmful invaders out of the brain. The barrier’s permeability increases with age — a deterioration scientists believe is linked to dementia.
Dr. Danny Wang’s two-group team will use two innovative imaging methods to examine small blood vessels in the brain. One group, led by Wang, will use magnetic resonance imaging to measure blood vessel stiffness. Inflexible arteries can be a sign of high blood pressure and other blood vessel conditions.
The other USC group, led by Amir Kashani, will use a new type of imaging called Optical Coherence Tomography Angiography. It involves looking through the eye’s retina to observe capillaries and small arteries in the brain. This approach is so powerful that researchers can see objects a tenth of the diameter of a strand of hair.
“Typically, it’s difficult to look directly at small vessels in the brain, but OCTA [the retina imaging technique] is a relatively cheap and accessible way to see arterials and capillaries in great detail,” Wang said. “As a result, there has been growing interest in using this technology to find early markers of dementia.”
The second phase of the NIH project, which began this year, involves consortium scientists validating promising biomarkers that other members found, and preparing them for use in clinical trials.
Drawing from a pool of 6,200 Latinos — a population historically underrepresented in aging research — researchers hope to have a suite of biomarkers ready for trials soon.
Ultimately, the discoveries the consortium makes are expected to lead to new treatments for Alzheimer’s and vascular dementia, a condition that often occurs in parallel with Alzheimer’s.





