Memory, Cognition in Mice with Alzheimer’s Improve When Inflammatory Cells Reduced, Researchers Say
Written by |
Researchers have successfully reduced the levels of inflammatory cells in the central nervous system linked to inflammation using pharmacological drugs. This decrease translated into improved memory, cognition, and neuronal survival in mouse models of Alzheimer’s disease.
The research paper, “Eliminating microglia in Alzheimer’s mice prevents neuronal loss without modulating amyloid-β pathology,” was published in the journal Brain.
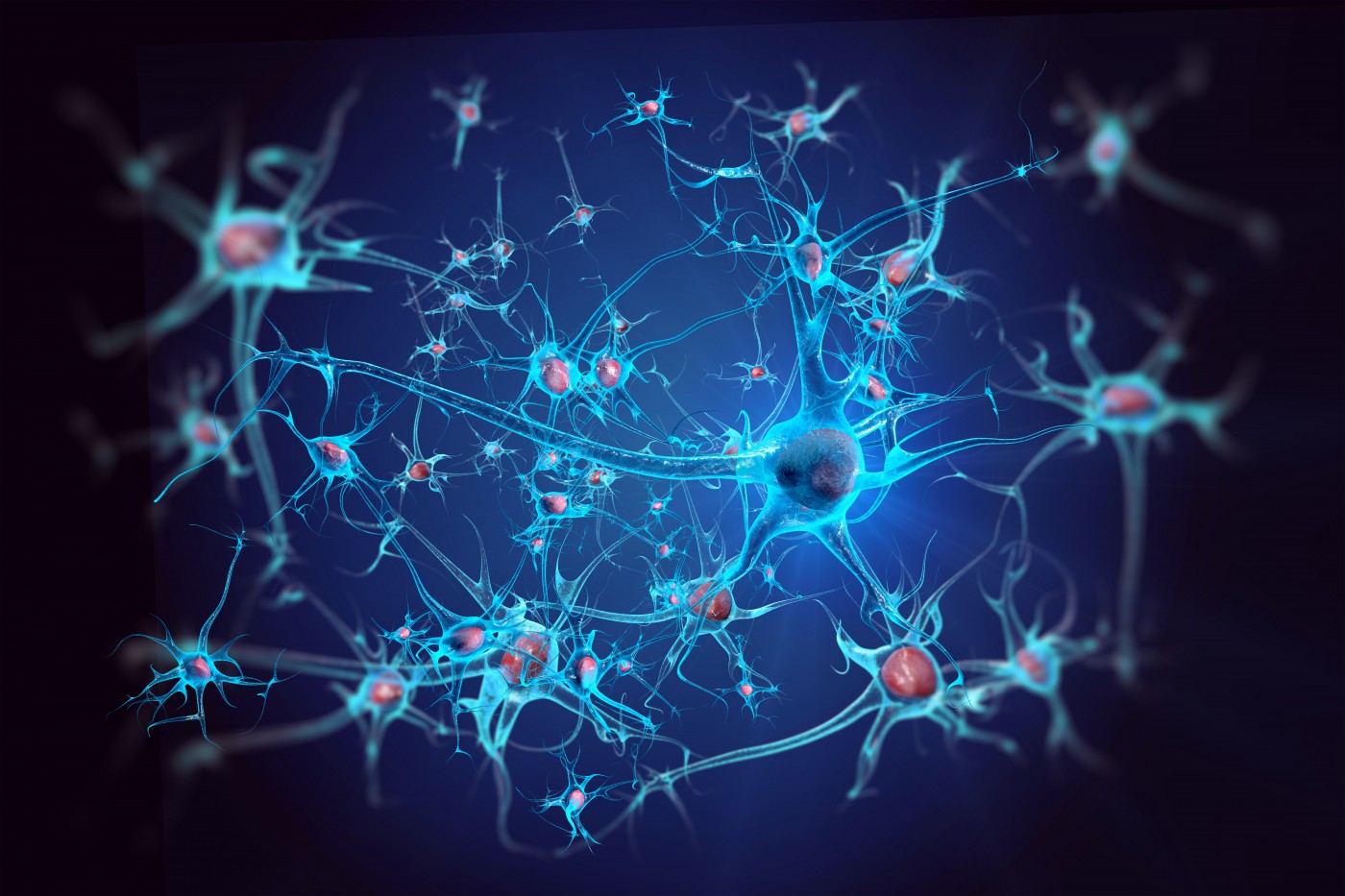
Neuroinflammation, along with amyloid-β plaque and tau neurofibrillary tangle deposition, is considered a key hallmark of Alzheimer’s disease. This inflammation is attributed to reactive astrocytes and abnormally activated microglial cells, which in normal circumstances act as the main immune defenses in the central nervous system, but in Alzheimer’s patients, turn against healthy tissue and are present in high levels among amyloid plaques, suggesting a possible implication of these cells in Alzheimer’s development.
In healthy mice, microglia depend on colony-stimulating factor 1 receptor (CSF1R) signaling for survival. Earlier research revealed that pharmacological inhibition of this receptor leads to the rapid elimination of most microglial cells in the central nervous system.
Researchers at the University of California, Irvine (UCI), studied whether activated microglial cells in Alzheimer’s disease are also dependent on this receptor and, if so, how they contribute to disease development.
Researchers treated mouse models of Alzheimer’s with a small molecule, pexidartinib (PLX3397), a selective CSF1R inhibitor that is currently in several Phase 2 oncology studies and a Phase 3 clinical trial to treat benign neoplasm of the joints. One month after treatment, about 80 percent of microglial cells were eliminated. This did not alter amyloid or plaque levels in mice brains, but it did prevent neuronal death, reduced overall neuroinflammation, and improved behavioral patterns, primarily memory and cognition.
“Our findings demonstrate the critical role that inflammation plays in Alzheimer’s-related memory and cognitive losses,” Kim Green, assistant professor of neurobiology amd behavior at UCI, said in a news release. “While we were successful in removing the elevated microglia resulting from beta-amyloid, further research is required to better understand the link among beta-amyloid, inflammation and neurodegeneration in Alzheimer’s.”
The results from UCI indicate microglia cells contribute to disease pathogenesis and could be a potential target for therapeutic approaches to treat Alzheimer’s disease.





