Monocytes in Human Umbilical Cord Blood Improve Alzheimer’s Cognitive Deficits
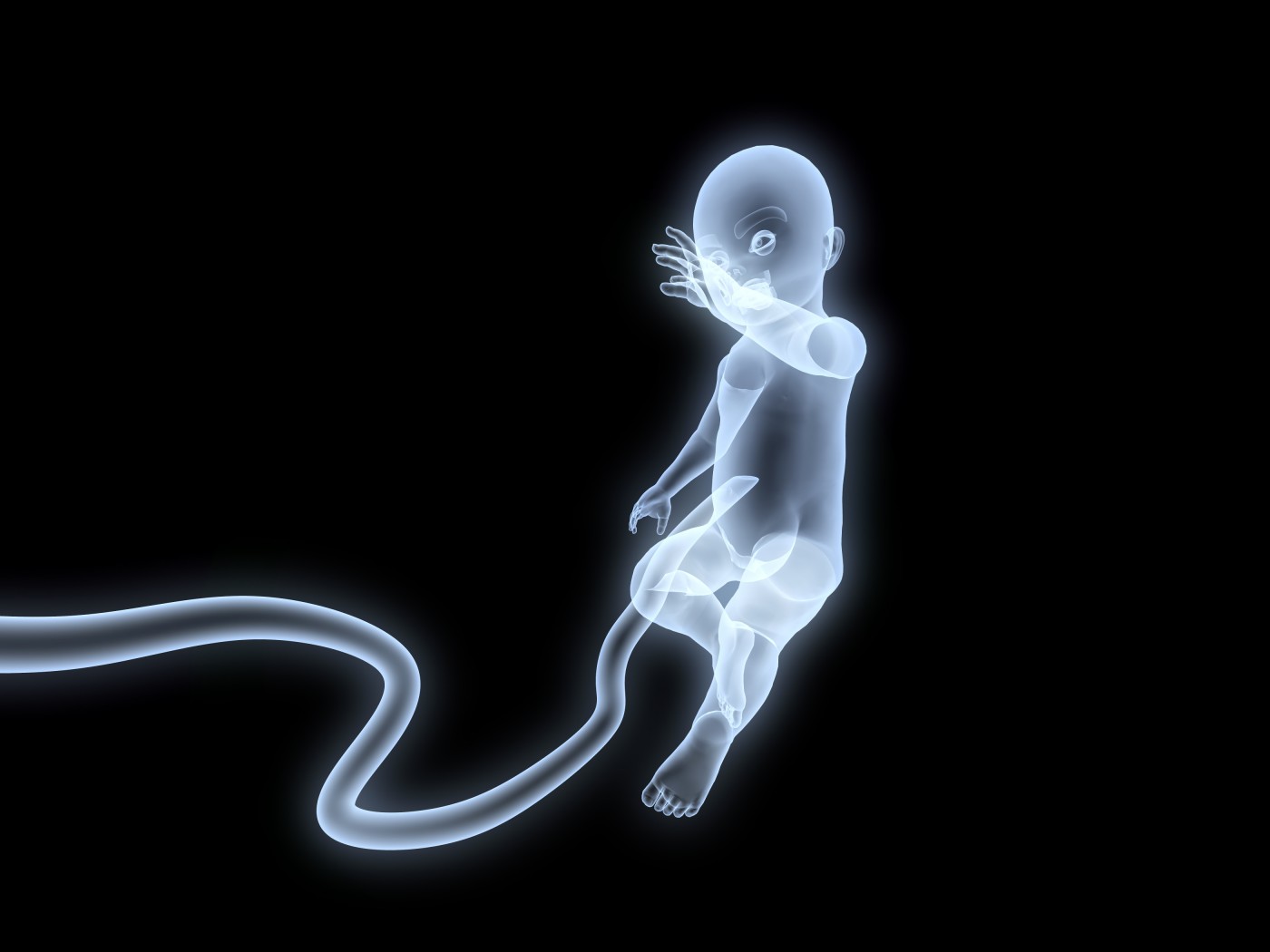
In a new study entitled “Human umbilical cord blood-derived monocytes improve cognitive deficits and reduce ß-amyloid pathology in PSAPP mice” an international team of scientists showed that infusion of human umbilical cord blood cells (HUCBCs) into a mice model of Alzheimer’s disease improves animals’ cognitive performance by clearing amyloid-beta (Aβ) plaques. They discovered that immune cells called monocytes, which are present in HUCBCs infusion are the key players responsible for this improved phenotype. The study will be published in the journal Cell Transplantation.
Currently affecting approximately 26 million people worldwide, Alzheimer’s disease (AD) is still without an effective treatment, with current medicines just ameliorating disease symptoms but not preventing disease progression. Recent studies with AD animal models have shown that HUCBCs transplantation reduces the effects of amyloid-beta (Aβ) plaques, the disease hallmark and key event responsible for neuronal death and dementia. Notably, however, the mechanism behind such phenotype is not known.
In this study a team of American, Chinese, and Japanese scientists tackled this mechanism and hypothesized that immune cells present in umbilical cords’ blood could play a role in Aβ plaque clearance. They specifically focused on monocytes (key players of the immune system in fighting infections and clearing foreign material) that belong to a wide family of cells called peripheral blood mononuclear cells (MNCs).
Study lead author Dr. Donna Darlington of the Rashid Laboratory for Developmental Neurobiology at the Silver Child Development Center, University of South Florida, noted, “We previously reported that HUCBCs modulated inflammation, diminished Aβ pathology, and reduced behavioral deficits in mice modeled with AD. In this study, we attempted to determine which MNC population was conferring these effects and to determine the mechanism by which these effects occur.”
The team treated AD mice with a monthly infusion of peripheral HUCBC-derived monocytes over a period of 2 and 4 months. The mice were then analyzed for behavioral changes, together with biochemical and histological analyses. The team discovered that monocytes derived from HUCBCs effective phagocytized and cleared Aβ aggregates, and also improved mice cognitive capacities, specifically learning, memory and motor function.
The study findings are key in AD research, as Dr. Shinn-Zong Lin, Vice Superintendent for the Center of Neuropsychiatry, Professor of Neurosurgery at China Medical University Hospital, and Co Editor-in-Chief for Cell Transplantation highlighted, “This study contributes insight into the possible mechanisms by which monocytes exert therapeutic effects. Future studies should weigh the benefits of using MNCs in cell therapy versus the possible detrimental effects, such as secretion of neurotoxic, inflammatory factors. The effectiveness of using MNCs in human AD patients should also be validated, as it has been a matter of conjecture.”






