Neuroinflammation in Alzheimer’s Is Again a Therapy Target
Written by |
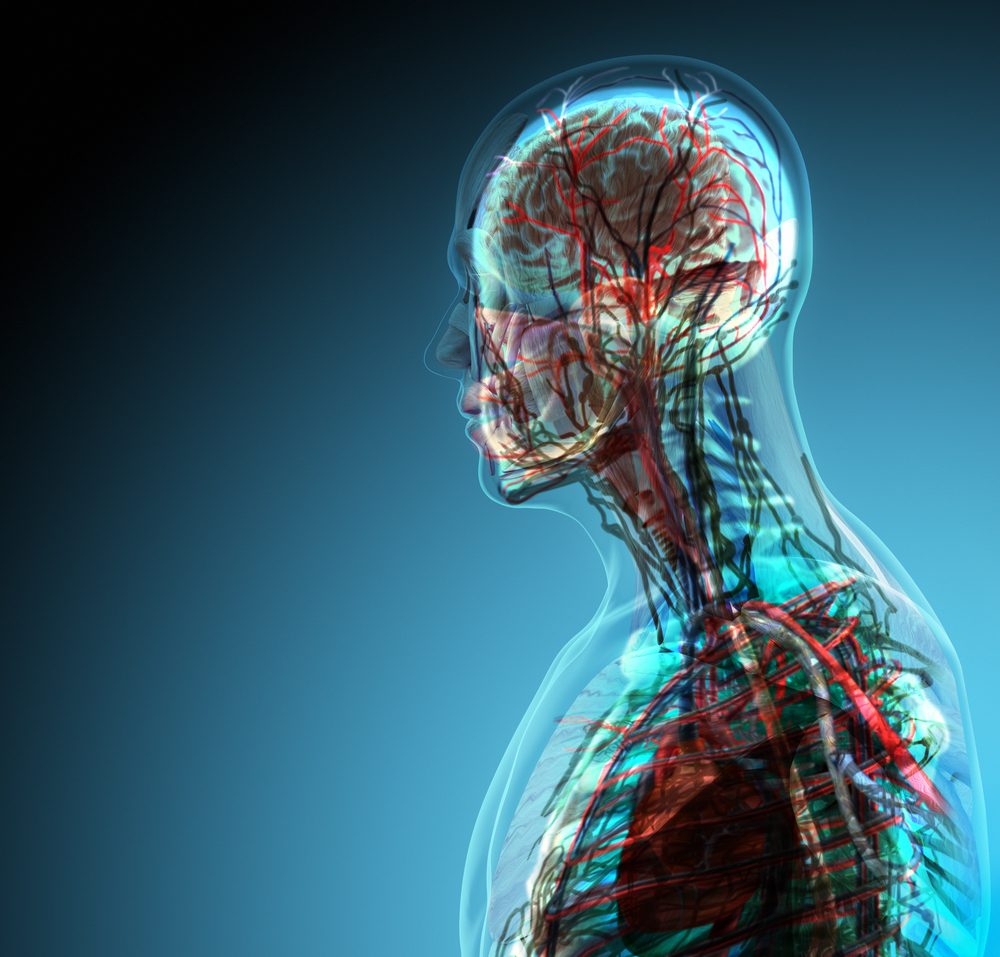
Neuroinflammation in the central nervous system is a known key event in Alzheimer’s pathogenesis and has long been proposed as a therapeutic target, but studies conducted in the early 2000s of potential anti-inflammatory treatments didn’t produce the hoped for outcomes.
Now a renewed interest is emerging in Alzheimer’s disease (AD) treatments targeting neuroinflammation, still a key marker with patients expressing high levels of inflammatory mediators close to beta-amyloid peptide deposits and neurofibrillary tangles, both associated with neurodegeneration.
“The field languished for at least a decade, until three years ago when intriguing findings about genetic risks for Alzheimer’s disease clustering around the innate immune system began to emerge, pointing to defects driving pathology,” Richard Margolin, MD, of CereSpir Inc., a pharmaceutical company developing new treatments for Alzheimers’s, said in a press release. Today, “[t]he study of neuroinflammation in AD is expanding by leaps and bounds.”
Novel results presented at the recent 8th lnternational Conference on Clinical Trials for Alzheimer’s Disease (CTAD) focused on two key cells of the innate immune system in the brain: astrocytes and microglia. Responsible for producing cytokines and engulfing injured or dead cells, debris, and toxins (a process known as phagocytosis), microglia cells become dysfunctional as Alzheimer’s disease progresses, releasing tissue-destructive cytokines.
Researchers at of CereSpir, and elsewhere, are continuing to rise to the challenge. As Dr. Margolin noted, “One strategy is to reduce cytokine production, but our approach is to pair that with enhancement of phagocytosis, because we think both are important and the combination could be synergistic. Preclinical studies showed beneficial effects for our drug CSP-1103 on both properties, and cytokine reductions were also seen in healthy volunteers and patients with mild cognitive impairment.”
The team at CereSpir wants to better understand why previous anti-inflammatory trials failed as it plans for a first late-stage trial of CSP-1103 in Alzheimer’s patients with mild cognitive impairment.
“Our trial will use an adaptive design because that approach enables a certain degree of flexibility, for example, in determining the final sample size for a trial. Regulatorily acceptable adaptive designs are attractive in late-stage development because they can potentially help accelerate the process, which is very important, given the long treatment periods required at this time for disease-modifying AD drugs,” Dr. Margolin said.





