Improved Brain Immunotherapy Delivery Strategy Uses Brain’s Natural Plumbing System, Study Reports
Written by |
A new approach for delivering antibody-based therapeutics to the brain by exploiting the fluid surrounding the brain’s blood vessels was proposed in a recent preclinical study.
This improved brain immunotherapy delivery strategy has implications for treating diseases of the brain and spinal cord, including Alzheimer’s, Parkinson’s, amyotrophic lateral sclerosis (ALS), frontotemporal dementia, and certain cancers.
The study, “Transcranial optical imaging reveals a pathway for optimizing the delivery of immunotherapeutics to the brain,” was published in JCI Insight.
Therapeutic antibodies are most commonly delivered directly into a vein due to the invasiveness and higher degree of complications associated with injections to the cerebrospinal fluid (CSF) — the fluid found inside the brain.
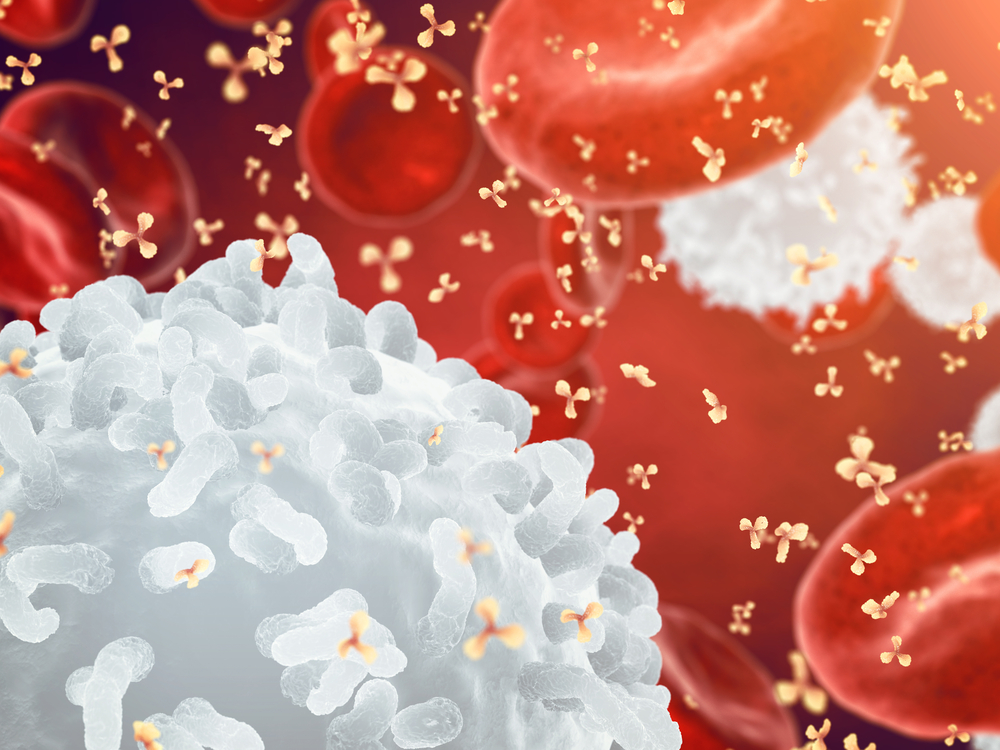
However, improving the delivery of therapeutics to the brain has proven to be a significant clinical challenge, especially in the case of immunotherapy — the treatment of disease by exploiting the immune system with antibodies.
Researchers think that the poor penetration of therapeutic immunotherapy to the brain is due to the blockage of antibodies by the blood-brain barrier and, therefore, limited target engagement. The blood-brain barrier is a semipermeable membrane that separates the blood from the cerebrospinal fluid and protects the brain from the outside environment.
Arguably the most notable application of brain immunotherapy has been applied to Alzheimer’s in efforts to enhance the clearance of amyloid-beta — the main component of the amyloid plaques crucially involved in disease development — from the brains of mice.
However, the results of brain immunotherapy clinical trials in people have been unimpressive and inundated by adverse events to patients after treatment.
Researchers at the University of Rochester Medical Center explored a specific pathway known as the glymphatic system to find out if it could represent a new strategy for improving the penetration of therapeutic antibodies to the central nervous system (CNS).
The glymphatic system, discovered by the same team in 2012, is a functional waste clearance pathway for the CNS — it works as the brain’s unique method to remove waste. It consists of a “plumbing system” that takes advantage of the brain’s blood vessels and pumps cerebral spinal fluid through the brain’s tissue, flushing away waste.
This system is highly active during sleep, clearing away toxins responsible for Alzheimer’s disease and other neurological disorders.
Researchers found they could exploit the glymphatic system to effectively deliver antibodies to the CSF.
Using a mouse model of Alzheimer’s disease, the team administered antibodies against amyloid-beta directly into the CSF. They then injected the animals with a solution called hypertonic saline, which is commonly used to reduce intracranial pressure on patients with traumatic brain injury.
This solution triggers an ion imbalance, pulling CSF out of the brain and stimulating the glymphatic system to deliver new CSF, together with the antibody, to take its place.
Importantly, delivery of amyloid-beta antibodies using the glymphatic system resulted in a fivefold increase for targeting amyloid-beta plaques over existing methodologies.
Therefore, the manipulation of glymphatic activity may represent a new strategy for improving the penetration of therapeutic antibodies to treat CNS diseases with brain immunotherapy.
The team also developed a transcranial optical imaging approach that enabled them to noninvasively and dynamically measure the transport and proliferation of antibodies into the brains of the animals.
“We obtained brain-wide imaging of CSF tracers, in contrast to the narrow field visualized by 2-photon microscopy, while obtaining spatial and temporal resolution that is not attainable with MRI [magnetic resonance imaging],” the researchers wrote.
“Our study … used substantially less antibody than required in previous studies, while achieving greater target engagement. Future studies should aim to determine if long-term increased plaque engagement can reduce plaque burden,” they concluded.





