Nitric Oxide Flips a Switch in Alzheimer’s Disease
Written by |
 Researchers at Massachusetts General Hospital (MGH) are looking to flip the molecular switch for inflammatory diseases such as Alzheimer’s to the “off” position. Masao Kaneki, MD, PhD, in the Department of Anesthesia, Critical Care, and Pain Medicine at MGH, discovered that nitric oxide acts on the protein SIRT1, leading to inflammation and cell death in multiple cellular and animal models.
Researchers at Massachusetts General Hospital (MGH) are looking to flip the molecular switch for inflammatory diseases such as Alzheimer’s to the “off” position. Masao Kaneki, MD, PhD, in the Department of Anesthesia, Critical Care, and Pain Medicine at MGH, discovered that nitric oxide acts on the protein SIRT1, leading to inflammation and cell death in multiple cellular and animal models.
“Since different pathological mechanisms have been identified for diseases like type 2 diabetes, atherosclerosis, and Parkinson’s disease, it has been assumed that therapeutic strategies for those conditions should also differ,” said Dr. Kaneki in a news release. “In contrast, our findings identified nitric oxide-mediated inactivation of SIRT1–believed to be a longevity gene–as a hub of the inflammatory spiral common to many aging-related diseases, clarifying a new preventive molecular target.”
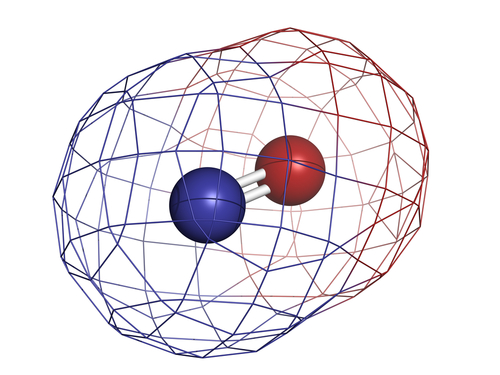
Under normal conditions, nitric oxide is a molecule that is integral to processes such as vasodilation. During inflammation an enzyme called inducible nitric oxide synthase (iNOS) produces an abundance of nitric oxide, allowing aberrant protein modification and transcription factor activation that eventually leads to cell death, disease, and signs of aging.
Previous reports have shown a role for nitric oxide in Alzheimer’s, diabetes, atherosclerosis, and many other aging-related disorders involving chronic inflammation. Dr. Kaneki’s report investigated a potential mechanism for nitric oxide-mediated inflammatory effects. Dr. Kaneki and the rest of his team at MGH and collaborative institutions published the results in “Inflammatory Stimuli Induce Inhibitory S-nitrosylation of the Deacetylase SIRT1 to Increase Acetylation and Activation of p53 and p65,” in Science Signaling.
Experiments showed nitric oxide caused S-nitrosylation of SIRT1, disallowing SIRT1 to bind zinc and consequently allowing transcription factors p53 and NF-kappaB to become active. These transcription factors are known to cause cell death in response to damage.
The team was able to block iNOS and prevent the behavioral effects in Parkinson’s disease models. “We’re now trying to identify small molecules that will specifically inhibit S-nitrosylation of SIRT1 and related proteins and suppress this proinflammatory switch,” said Dr. Kaneki. This specificity will be important to proper treatment without side effects, as nitric oxide is required in the healthy state.
One intriguing aspect of the study is how the mechanism applies to more diseases than just Alzheimer’s. “Regardless of the original event that set off this process, once turned on by SIRT1 inactivation, the same cascade of enhanced inflammation and cell death leads to many different disorders,” explained Dr. Kaneki. “While we need to confirm that what we found in rodent models operates in human diseases, I believe this process plays an important role in the pathogenesis of conditions including obesity-related diabetes, atherosclerosis, Alzheimer’s disease, and the body’s response to major trauma.”





