Novel Mechanism Involving Beta-Amyloid Protein Linked to Alzheimer’s Disease
Written by |
An international team led by researchers at The Rockefeller University and Columbia University recently published in the journal Nature Medicine a novel mechanism through which it is possible to decrease the production of beta-amyloid protein, a key factor in Alzheimer’s disease development. The study is entitled “APP intracellular domain–WAVE1 pathway reduces amyloid-β production”.
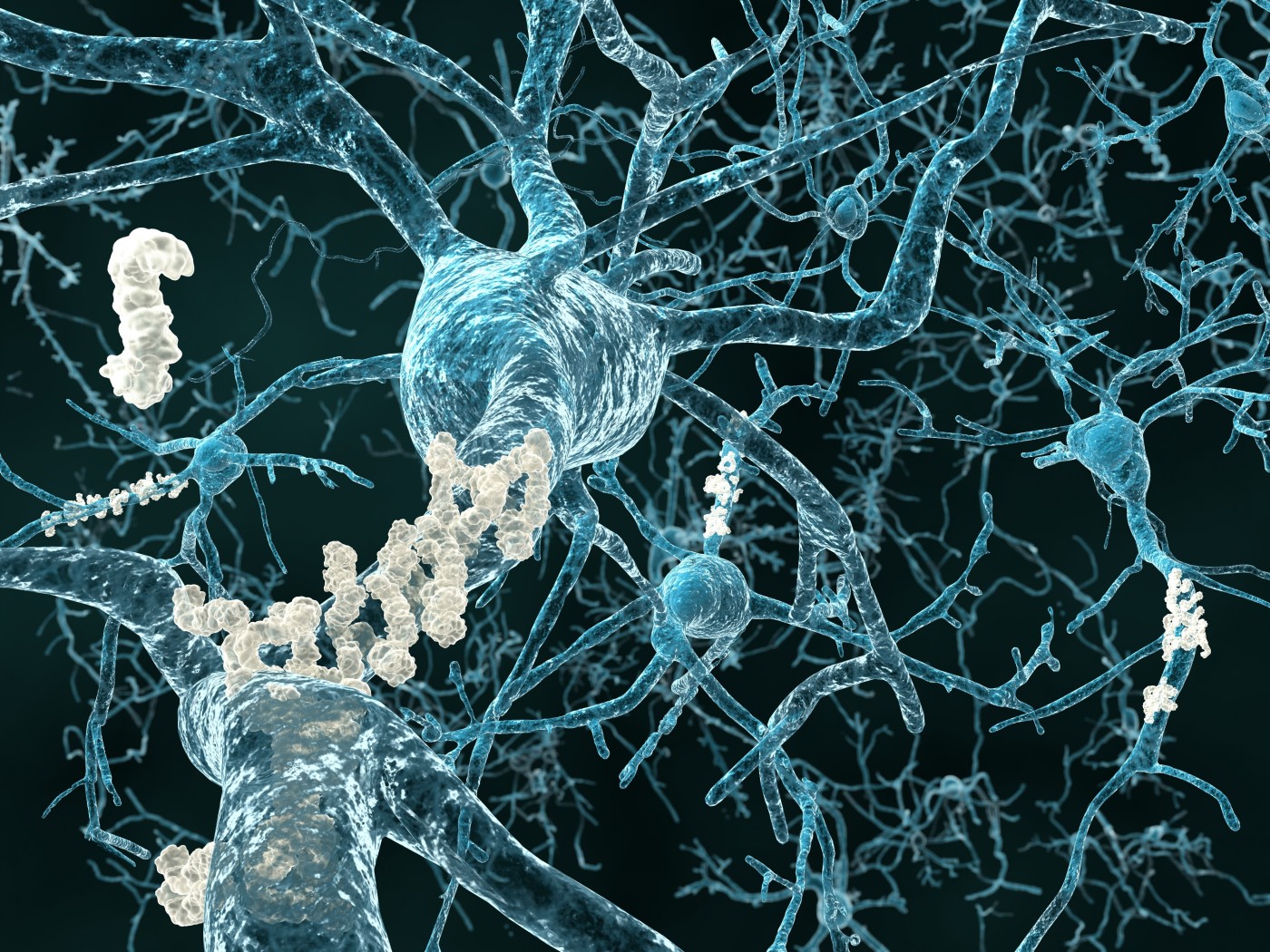
Alzheimer’s disease is a neurodegenerative disorder characterized by cognitive and behavioral problems. It is the most common form of dementia in the elderly with patients initially experiencing memory loss and confusion that gradually leads to behavior and personality changes, a decline in cognitive abilities and ultimately to severe loss of mental function. Alzheimer’s disease is characterized by the loss of neurons responsible for memory and learning, and brain formation of amyloid plaques containing aggregates of sticky beta-amyloid proteins. It is estimated that 44 million people worldwide suffer from Alzheimer’s or other form of dementia.
In the study, researchers investigated in more detail the pathways that lead to the generation and accumulation of beta-amyloid proteins.
The team found that the molecule that originates beta-amyloid, the amyloid precursor protein (APP), more exactly the intracellular domain of the protein (AICD), can downregulate the expression of a protein called WAVE1 in neuron cells, thereby limiting the production of beta-amyloid. This is a natural negative feedback mechanism to avoid over-production of beta-amyloid.
“Our discovery centers on a protein called WAVE1, which we found to be important in the production of amyloid-β. The reduction of WAVE1 appears to have a protective effect against the disease,” explained the study’s co-author Dr. Paul Greengard in a news release. “When levels of amyloid-β rise, there is an accompanying increase in another molecule, AICD, which reduces the expression of WAVE1. This has the effect of reducing the production of amyloid-β.”
“The result is a negative feedback loop,” added the study’s senior author Dr. Yong Kim. “More amyloid-β means more AICD. Our experiments reveal that AICD travels into the nucleus where it reduces the expression of WAVE1. (…) In Alzheimer’s disease, this negative feedback appears to lose its protective effect, and the next step for us is to figure out how.”
Researchers reported that a decrease on WAVE1 levels in neuron cells decreased the proper processing of APP and its cell-surface expression, leading to a reduction in beta-amyloid production. Interestingly, mouse models of Alzheimer’s disease exhibit an unusually low WAVE1 expression. In these animals, further reduction of WAVE1 expression led to a dramatic decrease in beta-amyloid levels and, importantly, to a better performance on memory tests.
A decreased expression of WAVE1 mRNA has also been observed in the brains of Alzheimer’s patients, suggesting that the findings may have clinical relevance for humans.
The research team concluded that there is a negative feedback circuit that controls the production of beta-amyloid proteins, and suggests that this novel mechanism may offer new therapeutic approaches for Alzheimer’s disease.
“By targeting steps within this newly discovered pathway,” concluded Dr. Greengard, “it may be possible to develop drugs to reduce amyloid-β that potentially could be used to either treat or prevent Alzheimer’s disease.”





