Phase 3 Trials of Gantenerumab Likely to Decide Clinical Benefit, Roche Says in Interview
Roche soon will start two Phase 3 trials testing gantenerumab, its amyloid-targeting treatment candidate, in prodromal, or early, Alzheimer’s patients.
Each plans to enroll 750 people, ages 50 to 90, and will judge gantenerumab’s effectiveness and potential clinical benefit by looking at changes in dementia and amyloid plaque load in the brain.
The Phase 3 trials — GRADUATE1 (NCT03444870) and GRADUATE2 (NCT03443973) — will run for two years and be conducted at sites across the U.S, Canada, Europe, South America, Australia, and Asia.
“We haven’t published an exact date, but we’re definitely about to start these studies soon,” Rachelle Doody, MD, Roche’s global head of Neurodegeneration, said in an interview with Alzheimer’s News Today.
Patients will receive monthly, subcutaneous (under the skin) doses of gantenerumab, which will be titrated, or gradually increased, every three months. “The most important thing to realize about this titration is that it’s the same for all patients, regardless of their APOE genotype,” Doody said. The combination of the two APOE gene copies determines the APOE genotype, a well-known risk factor for Alzheimer’s.
The studies will be highly similar — same treatment, dosing, and outcome measures — to comply with US. Food and Drug Administration requirements that study results be replicated to ensure any signs of robust clinical benefit are real. Duplication is also an essential step to possible approval.
“It’s very common that, in late-stage development in Alzheimer’s disease, you have two very similar studies. We’re simply doing the two studies at the same time because we want to save time,” Doody said.
Learning from past efforts
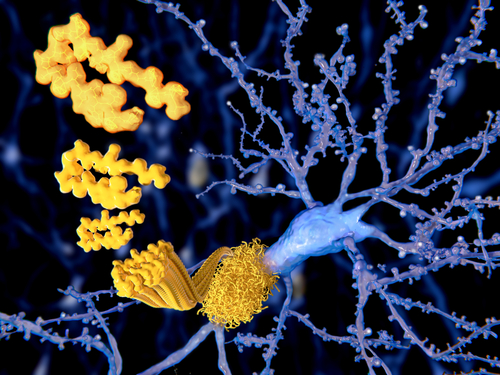
Gantenerumab is a fully human antibody that binds to aggregated beta-amyloid, a protein that accumulates in neurons and is the main component of the senile plaques characteristic of Alzheimer’s.
Its development started about a decade ago, and included a wide range of preclinical and clinical studies. Among them are Scarlet RoAD — first a Phase 2 study, and later a Phase 3 (NCT01224106) — and the Marguerite RoAD Phase 3 trial (NCT02051608) in patients with presymptomatic or mild Alzheimer’s. As in the GRADUATE studies, gantenerumab was given monthly under the skin.
Roche stopped Scarlet RoAD in 2014, based on an independent analysis suggesting it would be futile to continue the study as designed. No improvements in cognition or function were expected over placebo. “We decided that [gantenerumab’s dose] was too low in our early studies,” Doody said.
Researchers analyzed the data gathered since its 2010 start, however, and reported in 2015 that positron emission tomography (PET) imaging scans showed patients exposed to the higher dose of gantenerumab (225 mg) had lower levels of amyloid at one year of treatment. Those with the fastest disease progression also showed a slowing in cognitive decline.
“The people in higher exposure group did better,” Doody said. “That was our first inkling that higher dose might be better.”
These findings prompted the company to convert both the Scarlet RoAD and Marguerite RoAD trials into open-label extension (OLE) studies, in which all were given gantenerumab. “In the OLE, we explored different dose regimens, titration regimens, to move up to the new dose that we now know we need,” Doody said.
Scientists created a mathematical model to predict the gantenerumb dose most likely to achieve a minimum 20% reduction in aggregated amyloid levels.
Roche presented data on gantenerumab’s development, dosing, route of delivery, and other results at the recent AAT-AD/PD Focus Meeting 2018, held in Turin, Italy.
“Optimizing the Gantenerumab Phase 3 Dosing Regimen Through PK/PD Modeling and Clinical Trial Simulation”, given by Carsten Hofmann, PhD, found 1,200 mg of the therapy was the safest and most effective dose for the GRADUATE Phase 3 trials.
Data demonstrated the likelihood of “very good reductions of amyloid at the higher dose,” Doody said.
That dose has since been lowered to 1,020 mg due to a more efficient reformulation of gantenerumab, she added.
OLE results presented in the study “Analysis of Factors and Methodologic Considerations Affecting Plaque Reduction Measures via PET in the Gantenerumab Open Label Extension Studies,” by Gregory Klein, PhD, further revealed a “lowering of amyloid on the whole group as an average,” irrespective of a patient’s amyloid levels at baseline, Doody said, “meaning they got a high-enough dose for a long enough time.”
Such findings bolstered Roche’s decision to initiate the GRADUATE trials.
Doody noted that amyloid levels on PET scans do not correlate with Alzheimer’s stage because amyloid builds until it hits a disease threshold, which is around the level of prodromal Alzheimer’s. But a third of OLE study patients “lowered their amyloid below the threshold of positivity,” she said. “And that included people who started off with very high amyloid and people who didn’t.”
GRADUATE-1 and -2 will primarily assess against placebo changes in Clinical Dementia Rating Scale Sum of Boxes (CDR-SB) scores, much like Scarlet RoAD. Doody believes gantenerumab at high dose given in up-titration regimen could lead to “amyloid lowering [that] may correlate with clinical symptoms.”
“That’s exactly what these trials are designed to do — to see if people get better, to see if amyloid lowers, and to see if they correlate,” she added. “That’s something we all very much want to know.”
Safety and tolerability as goals
Researchers also sought to lessen as much as possible the risk of ARIA-E — brain imaging abnormalities suggestive of inflammation in areas with amyloid decrease.
By progressively increasing the dose, they expect to keep the ARIA-E rate at 25%, which contrasts to an estimated 60% had gantenerumab been dosed straight at the higher dose. As for symptomatic ARIA, data from the OLE studies — both expected to end in 2020 — showed a very low rate.
“The good thing about it is that is really very unusual, about 4% of all patients in the study,” Doody said. “So we think we have very good tolerability.”
Roche also presented data at Turin comparing different devices, kinds of deliveries, and ideal places for gantenerumab injections. The study “The Effect of Speed of Injection on Pain, Tolerability, Safety and Pharmacokinetics Following SC Administration of Gantenerumab,” presented by Agnes Portron, PharmD, reported that subcutaneous injection into the abdomen was safe and well-tolerated.
Precise injection sites for GRADUATE have yet to be decided, Doody said.
“We’re trying to optimize delivery,” she said. “How can we make this as easy as possible for people? … An optimization step done to make it as easy as possible for home administration, and we’re not there yet.”
Other current studies
An ongoing Phase 2/3 trial of familial Alzheimer’s (NCT01760005) is also testing gantenerumab, Eli Lilly‘s solanezumab and JNJ-54861911, developed by Janssen, in more than 400 people with mutations that put them at risk for Alzheimer’s. The treatment is being investigated by the Dominantly Inherited Alzheimer Network (DIAN), and is currently recruiting participants at sites across North and South America, Europe, and Australia.
Roche is also testing crenezumab, a monoclonal antibody that recognizes multiple forms of aggregated amyloid-beta, in several trials comparing the new molecule with placebo. These include:
- The CREAD Phase 3 study (NCT02670083) assessing the efficacy and safety of intravenous crenezumab in patients with early to mild Alzheimer’s over 100 weeks of treatment. It expects to conclude in July 2021.
- The CREAD 2 Phase 3 trial (NCT03114657) testing crenezumab in the same patient population for the same duration. Patients may also enter an open-label extension or a long-term follow-up period at treatment’s end. Enrollment of some 750 participants is now ongoing worldwide, and the study runs through October 2022.
- A Phase 1b trial (NCT02353598) evaluating the safety and tolerability of at least two dose levels of intravenous crenezumab in people with mild to moderate Alzheimer’s, expected to end by September 2023.
- A Phase 2 study (NCT01998841), anticipated to end in February 2022, testing the efficacy and safety of crenezumab given either intravenously or under the skin for at least 260 weeks in presymptomatic Alzheimer’s patients with the E280A mutation on the PSEN1 gene, the most common cause of familial early-onset Alzheimer’s.
‘Best target to start with’
The search for an Alzheimer’s treatment has been hampered by numerous setbacks, including ones just this year.
In January, Pfizer announced it was abandoning drug development for Alzheimer’s and Parkinson’s due to years of failure. The company decided to reallocate research money elsewhere.
Then Merck announced it was stopping its Phase 3 trial (NCT01953601) of verubecestat (MK-8931) in patients with early stage disease, likely for lack of effectiveness, in February.
Around the same time, Biogen announced it will recruit 510 more patients for its two Phase 3 studies — EMERGE (NCT02484547) and ENGAGE (NCT02477800) — on aducanumab (BIIB037), which also targets amyloid plaques in early Alzheimer’s patients, due to higher variability than assumed.
“Trials fail for many reasons,” Doody said. “They fail for reasons very specific to the exact molecule being tested, they fail for reasons that have to do with the conduct of the study, for reasons that have to do with the hypothesis.”
There’s many questions yet unanswered in a disease as complex as this one, she added. They include such basics as “whether amyloid is a good target for Alzheimer’s disease, or the best target for Alzheimer’s disease, or the only target for Alzheimer’s disease.”
Doody believes key events characterizing Alzheimer’s brain pathology, like amyloid deposition outside cells and neurofibrillary tangles within them, are the “place to start.”
Gantenerumab and crenezumab target amyloid differently. Roche is also testing another antibody against the tau protein, the main component of tangles that ultimately lead to neuronal death.
“We believe that the hypothesis has not been fully explored,” Doody said, “and that these are the best targets to start with.”






