Antibody Targeting Protein of Blood May Work Against Neurodegeneration, Study Reports
A newly developed antibody targeting a protein called fibrin was seen to prevent inflammation and oxidative stress induced by amyloid aggregates in the brains of a mouse model of Alzheimer’s disease.
These findings may pave the way for a new way of treating and preventing the neurodegeneration associated with Alzheimer’s and other neurological diseases.
The study, “Fibrin-targeting immunotherapy protects against neuroinflammation and neurodegeneration,” was published in the journal Nature Immunology.
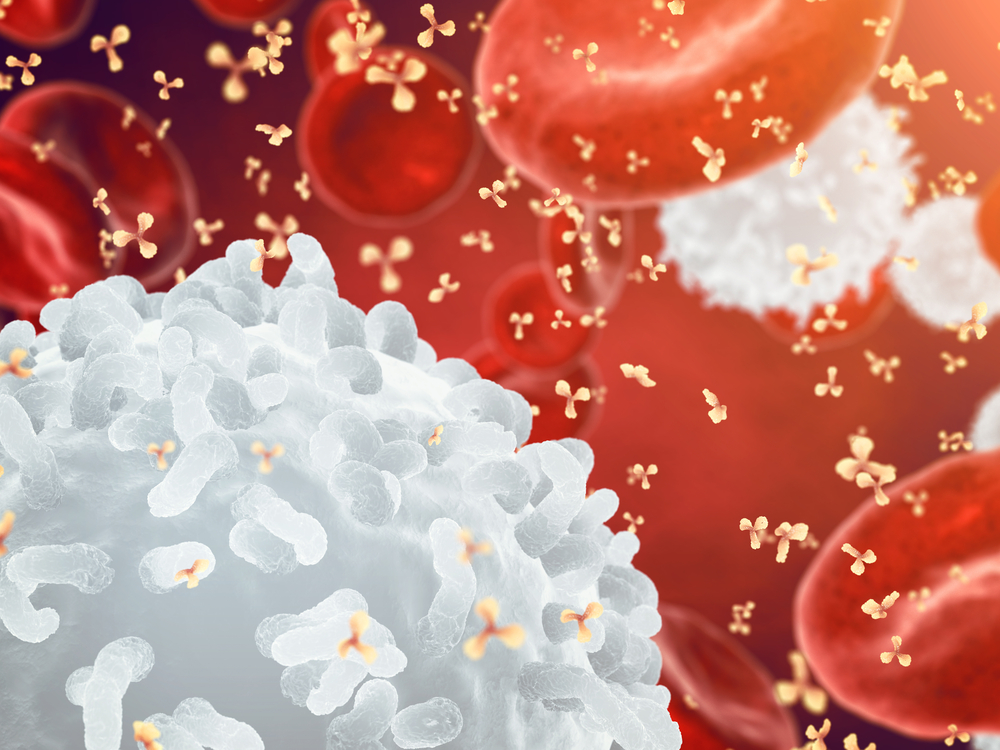
Abnormal activation of immune cells in the brain is known to contribute to the oxidative stress and cognitive decline linked to Alzheimer’s disease. Although little is still known about the signals that trigger immune cells, research suggests that disruption of the protective blood-brain barrier, and the consequent deposition of fibrin, are linked to the development of neurological diseases.
The blood-brain barrier consists of specialized cells that form a semi-permeable barrier that separates the brain from the circulatory system. Damage can allow fibrinogen, a soluble protein that’s also important to clotting of the blood, to leak into the central nervous system that includes the brain, where it is transformed into the insoluble protein fibrin.
Fibrinogen has been proposed as a biomarker for Alzheimer’s disease and mild cognitive impairment, with increased amounts of fibrinogen in the blood or cerebrospinal fluid being considered a predictor of brain atrophy.
Fibrin is known to activate immune cells and trigger pro-inflammatory responses, meaning that it can be a critical contributor for the underlying mechanisms of Alzheimer’s and other neurological disorders.
A team led by Gladstone Institutes’ researchers engineered an antibody — monoclonal antibody 5B8 — designed to bind to a specific part of the fibrin protein, a part that is known to bind to and activate immune cells in the brain.
“We have developed a monoclonal antibody to target a major culprit in the blood that damages the brain,” Katerina Akassoglou, PhD, a professor at University of California San Francisco and the study’s senior author, said in a Gladstone Institutes’ press release written by Julie Langelier.
“Fibrin-targeting immunotherapy could protect the brain from the toxic effects of blood leakage and may also have beneficial effects in other organs affected by inflammatory conditions with vascular damage,” Akassoglou added.
The immunotherapy was seen to inhibit fibrin-induced activation of immune cells by about 87% in experimental cells, without affecting the ability of the blood to clot normally.
Researchers also tested this antibody in mice models of multiple sclerosis (MS) and Alzheimer’s disease, two neurological disorders in which fibrin is known to play a role.
In mice with an MS-like disease treated before disease symptoms were evident, the antibody was seen to delay the onset of motor symptoms compared to mice treated with a placebo. When administrated after the disease was established, the antibody reduced the severity of motor symptoms, with fewer treated mice showing paralysis.
In both experiments, the treatment was well tolerated by the animals, and inhibited fibrin-mediated activation of immune cells in the brain, oxidative stress, and prevented damage to myelin, the protective coating on nerve cell fibers that is a hallmark of MS.
In mice with established Alzheimer’s disease, treatment with the investigational immunotherapy found it can effectively prevent the loss of cholinergic nerve cells in the brain — an Alzheimer’s hallmark — and stop the activation of immune cells near amyloid aggregates.
The antibody was also seen to significantly change the signaling patterns in brain cells by inhibiting major pro-inflammatory pathways and oxidative stress signals, without significantly changing the number of amyloid plaques or immune cells.
These findings suggest that blocking fibrin-mediated signaling can suppress amyloid-induced neurodegeneration and reduce the levels of molecules that promote inflammation and oxidative stress in Alzheimer’s disease.
“Our study supports that vascular damage leading to immune-driven neurodegeneration may be a common thread between diseases of different etiologies with blood-brain barrier leaks,” Akassoglou said. “Targeting fibrin with immunotherapy is a new approach that could be used to test the therapeutic benefits of suppressing this pathogenic mechanism in multiple disease contexts.”
The team is now planning to develop a version of this monoclonal antibody that could be used in people for possible testing in trials.






